mell & taste disorders are common in the general population, with loss of smell occurring more frequently.
The tongue can detect only sweet, salty, sour, bitter & ‘savoury’ (umami) tastes. Much of what is perceived as “taste” is actually “smell”. People who have taste problems often have a smell disorder that can make it hard to identify a food’s flavour. (Flavour is a combination of taste and smell [mainly] and texture & temperature).
Problems range from distorted taste (dysgeusia), reduced sense of taste (hypogeusia) to a complete loss of the sense of taste (ageusia). However, a complete inability to taste is rare.
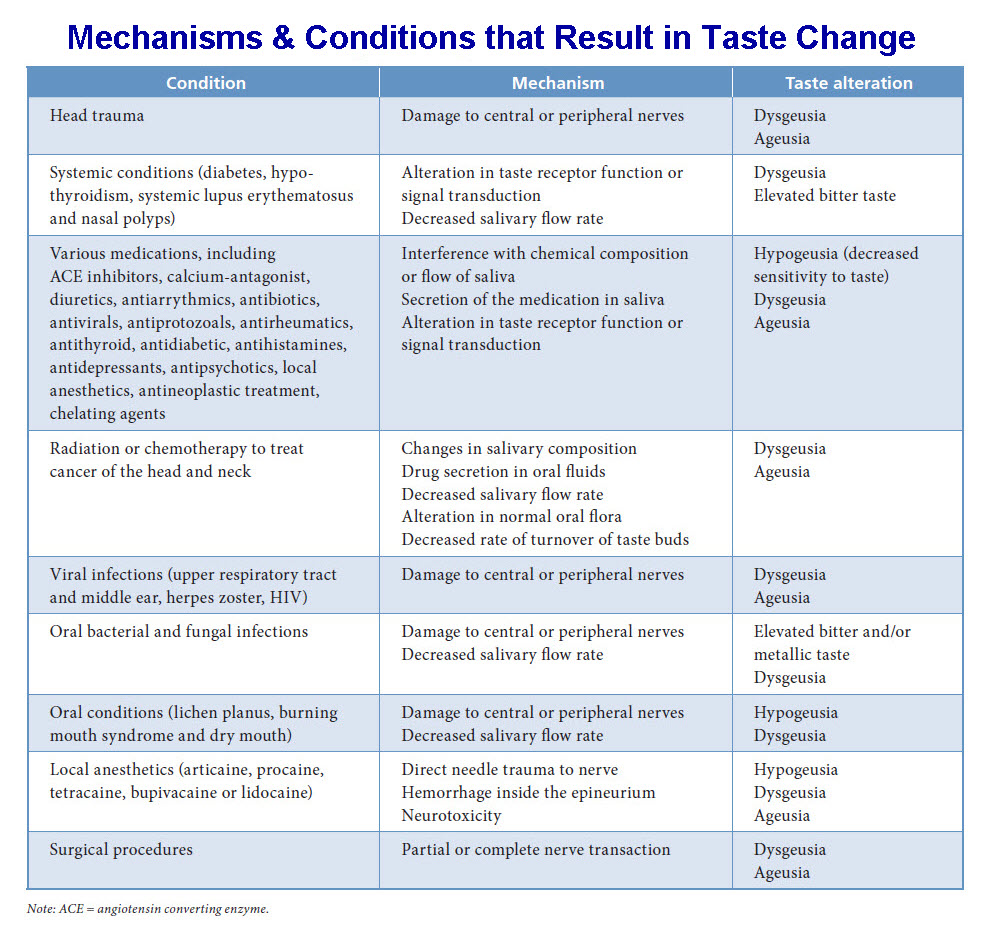
Taste problems can be caused by anything that interrupts the transfer of taste sensations to the brain (or vice versa) or by conditions that affect the way the brain interprets these sensations.
Advancing age has been associated with a natural impairment of smell and taste ability.
Types of Taste Loss
There are several ways of classifying taste disorders but the method most commonly applied in clinical practice, is to distinguish qualitative from quantitative taste disturbance as follows:
Dysgeusia: qualitative taste impairments, which include a multitude of complaints, such as metallic taste or permanent bitter, sour, salty or (even rarer) sweet taste.
Hypogeusia: a quantitative taste disturbance producing reduced taste function
Ageusia: a quantitative taste disturbance producing absence of taste.
Any of these can be triggered, lowered or unaffected by eating.
According to testing with taste strips, 5.3% of the people considered as healthy have hypogeusia and very few complete ageusia.
Other classifications are based on the anatomical site of the lesion (e.g. peripheral nerve lesion, brainstem lesion, thalamic or fronto-orbital lesion).
Causes
Taste sensation often decreases after age 60. Most often, salty and sweet tastes are lost first. Bitter and sour tastes last slightly longer.
Selected Possible Causes of Taste Disturbance
Common causes
- Oral & peri-oral infections (e.g. candidiasis, gingivitis, herpes simplex, periodontitis, sialadenitis)
- Nasal Infections / conditions such as the Common Cold, Flu, Pharyngitis and “Strep” throat, nasal polyps & sinusitis
- Bell’s palsy
- Oral appliances (e.g. dentures, filling materials, tooth prosthetics)
- Dental procedures (e.g. tooth extraction, root canal treatment)
- ENT procedures (middle ear surgery, tonsillectomy)
- Age
- Medications such as anti-thyroid drugs, captopril, griseofulvin, lithium, penicillamine, procarbazine, rifampin and some drugs used to treat cancer
Medications can be responsible for taste loss and should be reviewed in all patients with gustatory disturbance.
Xerostomia / excessive dryness of the oral cavity is a common side effect of a number of medications (e.g. anti-cholinergics, anti-depressants, anti-histamines) and disease states (e.g. Sj?gren’s syndrome, xerostomia, diabetes mellitus).
Less Common Causes
- Nutritional factors (e.g. vitamin deficiency [B3, B12], trace metal deficiency [zinc, copper], malnutrition, chronic renal failure, liver disease [including cirrhosis], cancer, AIDS)
- Tumour or lesions associated with taste pathways (e.g. oral cavity cancer, neoplasm of skull base)
- Head trauma / Injury to the mouth, nose or head
- Toxic chemical exposure (e.g. benzene, benzol, butyl acetate, carbon disulphide, chlorine, ethyl acetate, formaldehyde, hydrogen selenide, paint solvents, sulphuric acid, tri-chloro-ethylene)
- Industrial agent exposure (e.g. chromium, lead, copper)
- Radiation treatment of head and neck
Uncommon Causes
- Psychiatric conditions (e.g. depression, anorexia nervosa, bulimia)
- Epilepsy (gustatory aura)
- Migraine headache (gustatory aura)
- Sj?gren’s syndrome
- Multiple sclerosis
- Endocrine disorders (e.g. adreno-cortical insufficiency, Cushing’s syndrome, diabetes mellitus, hypo-thyroidism, pan-hypo-pituitarism, pseudo-hypo-parathyroidism, Kallmann’s syndrome, Turner’s syndrome)
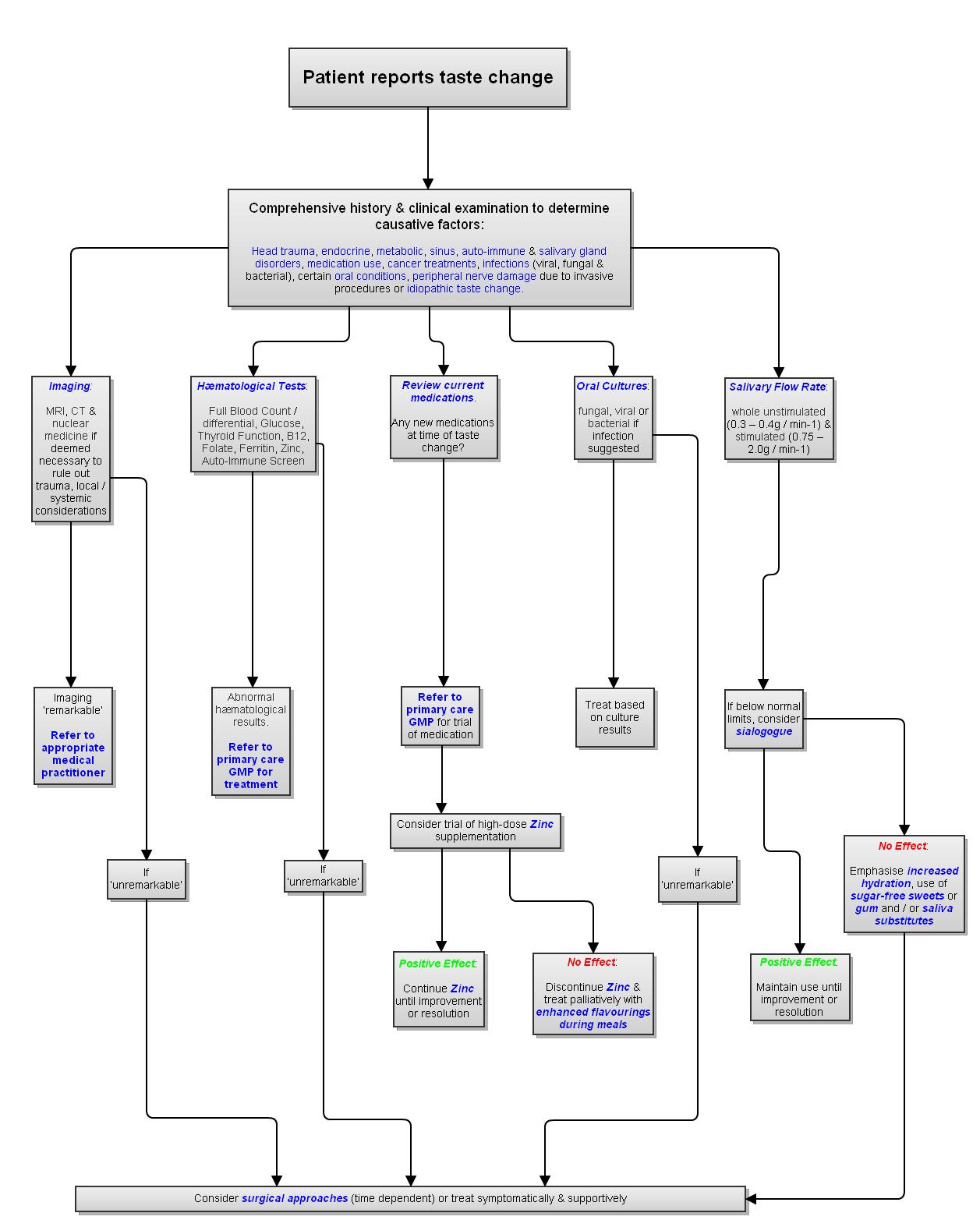
Step-by-Step Diagnostic Approach
The evaluation of a patient presenting with taste dysfunction comprises the patient’s history (including drug intake and nutritional elements), a detailed clinical examination (of the head, neck, ears, nose & mouth) and investigations to determine the underlying aetiology.
History
It is important to determine whether the patient can discern salt, sweet, bitter, sour and whether the taste disturbance is quantitative (hypogeusia / ageusia) or qualitative (dysgeusia).
It is important to determine whether the taste disturbance was acute in onset or was gradual. Acute taste loss is associated with iatrogenic (medically-related) or toxic causes whereas a more insidious onset may suggest a neurological (nerve dysfunction) or neoplastic (benign or malignant cancer) origin. Any concomitant loss of nasal function (i.e. smell & flavour) should also be ascertained.
A full medical history is taken including what medications / drugs the patient is on. Assessment of existing medical conditions (such as endocrinopathies or neurological conditions) can put the taste disturbance in context. A history of any precipitating event (such as recent trauma, medical procedure or radiotherapy) is needed as well.
Physical Examination
A thorough examination of the head, neck, mouth & ears should be performed to look for obstruction, inflammation, previous surgery & infection.
- A complete examination of the oral cavity (mouth) & naso-pharynx is done with particular attention to signs of previous surgery (such as missing 3rd molars [wisdom teeth] & tonsils).
Mucous membranes should be evaluated for dryness, leukoplakia (white patches) & exudates. The patient’s teeth and gingiv? (gums) should also be examined as severe dental caries (tooth decay), gingivitis (gum disease) & intra-oral abscess can result in a malodorous and caustic oral environment that disturbs the senses of smell and taste. Evidence of mucosal inflammation suggests possible nutritional deficiencies (such as chronic iron, zinc or B12) or inflammatory process.
Oral candidal infections in immuno-compromised patients (e.g., those who have received chemotherapy or who have AIDS) can produce white patches or diffuse erythema (redness). Viral infections (e.g. herpes simplex virus, coxsackie virus) tend to cause the development of vesicles (blisters) with surrounding erythema, which then evolve into erosions or ulcers.
A dry mouth (xerostomia) is looked for – signs include angular cheilitis, cervical (around the ’neck’ of the tooth) dental decay, tooth loss & mucous threads.
- The ears should be checked for any otitis with discharge (serous otitis) such as otitis media or for any previous surgery.
- The eyes should be checked for any sign of dryness (xerophthalmia) such as kerato-conjunctivitis sicca.
- The neck should be checked for any previous neck surgery or thyroid enlargement..
The major salivary glands (the parotid & submandibular) should be checked for possible enlargement (suggestive of Sj?gren’s Syndrome [link to Sjoegren’s Syndrome webpage]).
Depending on the clinical history, a neurological examination may be warranted. This should include a careful evaluation of cranial nerve
Chemo-Sensory Gustatory Testing
It is difficult for patients to measure taste disturbances objectively, so chemical gustometry / electro-gustometry should be used.
Chemical Gustometry
Solutions of the 4 fundamental tastes (sweet, sour, sweet & bitter; occasionally, umami) are applied to the tongue surface.
Results are reported as any decrease of taste sensation on the area of the tongue tested.
Electro-Gustometry
An electrode is used to breakdown water (hydrolysis) in the saliva. This stimulates the taste buds eliciting a sour, sometimes metallic, taste recognised by the patient.
Results are reported as non-detectable or increased thresholds on the areas of the tongue tested.
Olfactory Testing
In most patients with taste disturbances, olfactory function should be assessed. This is more objective if tested than just asking the patient.
There are a number of validated olfactory testing methods (such as the Smell Identification Test, the Pocket Smell Test, the Brief Smell Identification Test and the Odor Threshold Test); these are all based on similar principles.
There are a number of validated olfactory testing methods (such as the Smell Identification Test, Pocket Smell Test, . The Brief Smell Identification Test and the Odor Threshold Test); these are all based on similar principles.
Laboratory Investigations
Clinical laboratory tests may be helpful in ruling out co-existing medical conditions suggested by the history & physical examination, such as infection, nutritional deficiency, allergy, diabetes mellitus & thyroid, liver or kidney disease (such as FBC, peripheral blood smear, serum ferritin, vitamins B12 & folate, zinc, thyroid function tests, liver function tests, oral glucose tolerance test, serum fasting morning glucose test, Ro-La antibodies & acetylcholine receptor antibody [if myasthenia gravis suspected]).
Imaging
When structural or inflammatory causes of smell or taste loss are suspected, imaging studies may be helpful in selected patients. However, all imaging techniques have limitations & negative tests cannot rule out structural lesions.
Computed tomographic (CT) scanning is the most useful technique for assessing skull fractures, intra-cranial bleeds, sub-dural h?matoma or areas of isch?mia. It also picks up well Alzheimer’s Disease, Multiple Sclerosis, sino-nasal tract inflammatory disorders.
The use of intravenous contrast media helps to better identify vascular lesions, tumours, abscess cavities & meningeal or para-meningeal processes.
MRI is superior to CT scanning in the evaluation of soft tissues but it poorly defines bony structures. MRI is the technique of choice for assessing the olfactory bulbs, olfactory tracts, facial nerve & intra-cranial causes of chemo-sensory dysfunction. It is also the preferred technique for evaluating the skull base for invasion by sino-nasal tumours. Gadolinium enhancement is useful for detecting dural or lepto-meningeal involvement at the skull base.
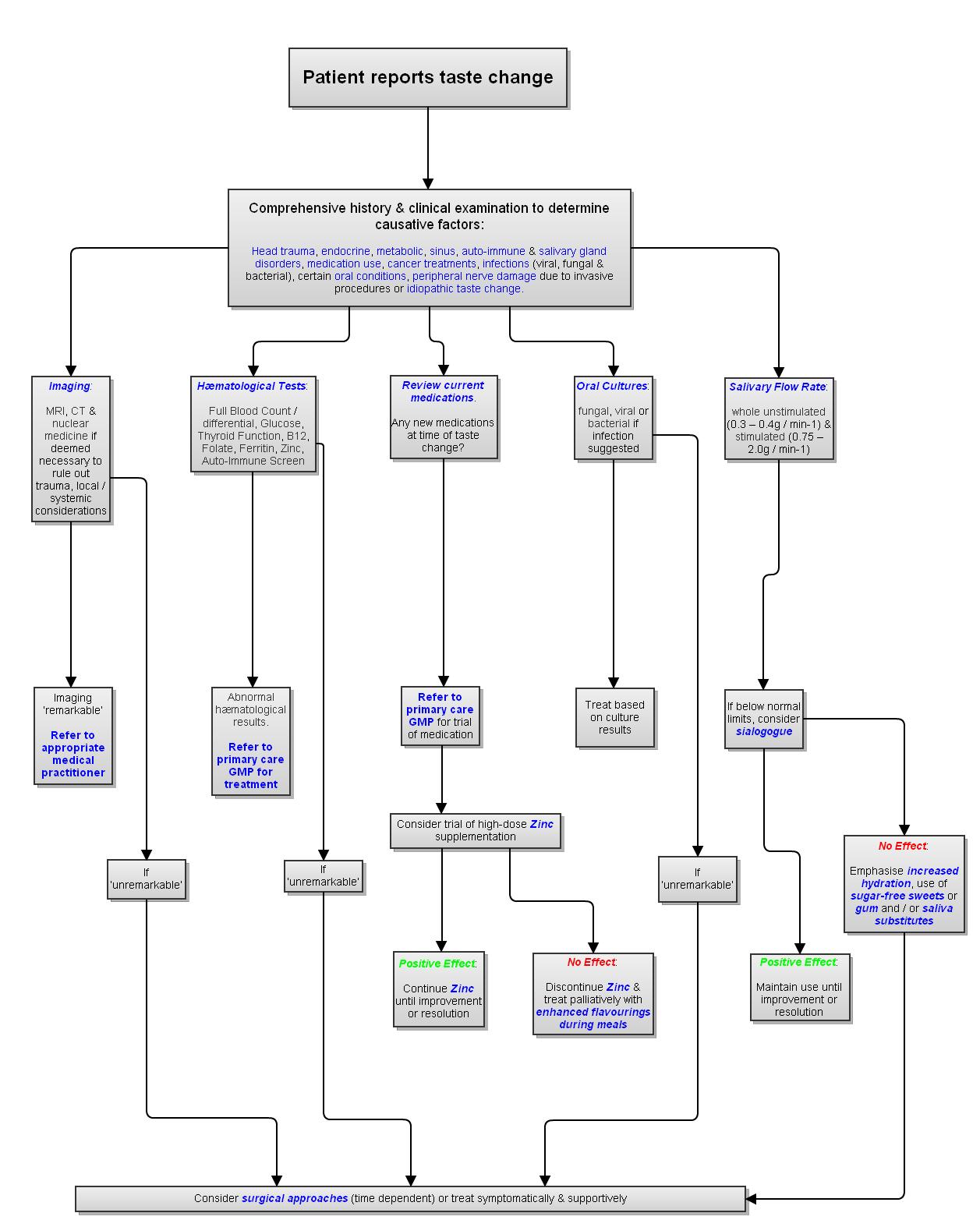
Treatment Algorithm for Taste Disturbances
Treatments
Many taste disorders (dysgeusias) resolve spontaneously within a few years of onset.
However, several immediate steps can be taken to help correct a taste disturbance. For example, some drug-related dysgeusias can be reversed with cessation of the offending drug.
Conditions such as radiation-induced xerostomia & Bell’s Palsy generally improve over time. An artificial saliva (e.g. Xerolube) may be helpful in patients with xerostomia.
The causes of olfactory dysfunction that are most amenable to treatment include obstructing polyps or other masses (treated by excision) and inflammation (treated with steroids).
Enhancement of food flavour & appearance can improve quality of life in patients with irreversible taste disturbance. Patients should be cautioned not to overindulge as compensation for the bland taste of food.
For example, patients with diabetes may need help in avoiding excessive sugar intake as an inappropriate way of improving food taste. Patients with taste disturbance should use measuring devices when cooking, not “cook by taste”. Optimising food texture, aroma, temperature and colour may improve the overall food experience when taste is limited.