An Introduction to Orofacial Pain
Many people who struggle with orofacial pain lack a clear understanding of how to get treatment.
The American Dental Association (ADA) has officially endorsed the specialty of Orofacial Pain. It has gained formal recognition by the ADA’s National Commission on Recognition of Dental Specialties and Certifying Boards in March 2020.
The rapidly evolving field of orofacial pain is an important dental specialty that crosses the lines of the medical and dental divide. Increased awareness of the specialty leads to improved access to care for many people suffering from these painful conditions. Early referral should improve the chance of successful treatment thereby reducing the risk of inappropriate or unnecessary dental treatment being carried out, and of the development of chronic pain.
There have been formal advanced Orofacial Pain training programs for decades. However, now with this formal recognition, the specialty can grow in terms of standards of education, development of best practices, and dedicated research efforts. Given the higher rates of jaw pain patients who visited dentists in the last year, obtaining experienced help for facial pain is vital. This will help the millions of Americans who suffer from chronic orofacial pain conditions.
What Is Orofacial Pain?
Orofacial Pain is the specialty of dentistry that encompasses the diagnosis, management, and treatment of pain disorders of the mouth, face, head, and neck. The Specialty of Orofacial Pain is dedicated to the evidence-based understanding of the underlying pathophysiology, etiology, prevention, and treatment of these disorders and improving access to interdisciplinary patient care, according to the AAOP.
Persistent orofacial pain refers to a group of chronic disorders affecting the face and mouth. It includes temporomandibular disorders, vascular disorders (such as migraine and cluster headaches), burning mouth syndrome, trigeminal neuralgia, persistent dentoalveolar pain disorder, and persistent idiopathic facial pain.
Orofacial Pain Specialist is defined as pain perceived in the face or oral cavity caused by diseases or disorders of regional structures or dysfunction of the nervous system or through referral from distant sources.
A rather profound advance in medical thinking came with the recognition that chronic pain, of itself, is considered a disorder. There is a complex interaction between biological, psychological, behavioral, and social factors that contribute to chronic pain disorders. This recognition gave rise to what is called the biopsychosocial model, one that uses an interdisciplinary approach to treating chronic pain, and it spans across the fields of both medicine and dentistry.
Furthermore, there is a bidirectional and mutually reinforcing dynamic between the neurobiological processing of pain in the central nervous system and in the peripheral tissues. The tissues that are involved include muscles, joints, nerves, or blood vessels.
Anatomy of Orofacial Pain Areas:
- Teeth
- Mouth
- Tongue
- Jaw
- Maxilla (upper jaw bone)
- Mandible (lower jaw bone)
- Temporomandibular joint (TMJ)
- Muscles of mastication
- Cervical muscles and joints
- Cranial nerves (especially the trigeminal nerve)
- Cranial vascular system
The implication of these facts put together is that when treating chronic orofacial pain, experts must be trained in both the medical and dental aspects of the disease. If a practitioner knows only the medical aspects of pain management, they will be unable to address the peripheral causes perpetuating the pain. Likewise, if a dentist does not understand the neurobiological and psychological aspects of chronic pain, they will not be able to address the central nervous systems components of orofacial pain.
Orofacial Pain Specialists Treat the Following Conditions
TMJ Disorders
- TMJ disc derangement
- TMJ degenerative disease
- Myofascial pain
Headaches
- Migraine headaches
- Tension-type headaches
- Cluster headaches
Neurological Disorders
- Trigeminal neuralgia
- Orofacial movement disorders
Orofacial Disorders
- Atypical facial pain
- Burning mouth syndrome
- Periodontal ligament strain
Sleep Disorders
- Sleep apnea
- Sleep bruxism
- Snoring
History of the Orofacial Pain Specialty
Why was a new Orofacial Pain Specialist designation needed?
The answer lies in the history of how medicine and dentistry became separate health professions. The beginnings of the medical and dental divide go back to the days of barbers and alchemists when certain practitioners developed distinctive techniques in treating teeth problems and wanted to distinguish themselves from other providers of care.
But while the craft of dentistry is centuries old, the profession of dentistry did not start until 1840, with the creation of the first dental college in Baltimore. This is when dentistry began to truly separate from the field of medicine and become distinct in practice, technique, and tradition.
Another major shift came with the rise of the health insurance system in the 1960s and 1970s when medical care was included, but dental problems were excluded. This further divided cultural thinking about medicine and dentistry, both for laymen and health professionals.
Yet while it seems natural today to think of medicine and dentistry as separate, the mouth and jaw are not separate from the brain and body. The historical divide between medicine and dentistry has created a lack of communication, consensus, and treatment standards for conditions that fall in the middle ground between the two fields, with orofacial pain conditions being a prime example.
To address this gap in knowledge and practice, the American Academy of Orofacial Pain was established in 1975. In the decades since, the field became more organized and its knowledge base more refined. While the first accredited orofacial pain program was created at the University of California, Los Angeles in 1996, formal recognition of the specialty only happened in 2020.
Recognition of this specialty solidifies another link between dentistry and medicine, acknowledging that the orofacial region, oral cavity, and masticatory system are an integral part of total patient care.” – Gary Heir, DMD, an internationally recognized expert on orofacial pain, on jada.org.
How TMJ Disorders Relate to Orofacial Pain
For years, patients have tried to find the correct practitioner for TMJ issues, usually finding themselves consulting with a dentist with no specialty training or an Ear Nose Throat (ENT) doctor with limited knowledge of TMJ issues. But TMJ disorders are squarely in the area of expertise of Orofacial Pain specialists. They are trained not only to treat the orthopedic problems of the TM joint, but also different types of muscle pain related to the TMJ complex.
The orthopedic problems of the TMJ include disc derangement, joint degeneration, and joint and muscle sprain strain (JAMSS). These are not always painful conditions, but the Orofacial Pain specialist is trained to treat these disorders.
The most common TMJ disorder is called myofascial pain (but is also referred to as myalgia). The current understanding of myofascial pain is that it is triggered by a cascade of events that usually start with an acute jaw injury or repetitive strain to the jaw muscles resulting in continuing muscle discomfort.
The sequence is as follows:
- Acute injury in the TMJ complex triggers a guarding reflex in the jaw muscles.
- Persistent muscle tension from guarding and clenching the teeth leads to tissue sensitization, muscle fatigue, and subsequently, increased pain signals to the central nervous system and brain.
- These persistent peripheral pain signals in the tissues induce a hyper-excitable state in the neurons of the central nervous system. This is process is called “central sensitization”.
- With “central sensitization”, there is hyperalgesia, tenderness, and referred pain.
According to MedCrave research, “32.7% of patients recognized a TMJ-related problem that affected their quality of life, while 67.3% suffering from TMD were unaware of their TMJ disorder. It affects 5-12% of the population and the peak age is 20-40 year.” Author Dr. Danya A Alhussini highlights in her October 8, 2017 Prevalence and awareness of temporomandibular joint disorders among patients article that the temporomandibular joint (TMJ) is one of the most complex joints in our bodies. Orofacial Pain specialists have many tools with which to treat TMJ disorders.
- With this increase in perceived pain signaling, the muscle guarding reflex remains activated, creating a vicious cycle of pain.
Orofacial Pain specialists have many tools with which to treat TMJ disorders.
Treatment options include:
- Self-management with exercises and cognitive-behavioral training
- Intraoral appliance therapy(mouthguards specifically designed for addressing specific TMJ disorders)
- Muscle injections with local anesthetic or Botox
- Pharmacological management
- Joint injections
- Nerve blocks
- Physical therapy
- Psychological therapy
TMJ surgery is rarely needed, but when it is, Orofacial Pain specialists are trained to consult with an Oral and Maxillofacial Surgeon. They help manage pain before and after surgery.
Headaches
Headaches are common and there are various types and causes, the most common primary types being tension, migraine, and cluster headaches.
Orofacial Pain specialists are trained to treat headaches and collaborate with neurologists. Most common primary headaches are related to the TMJ complex. In recognition of this, the International Association for Dental Research officially recognized Headache Attributed to Temporomandibular Disorders as its own diagnostic category. This is important because neurologists have little specialized training in the structure and function of the TMJ complex. Thus, they may not be experienced in treating headaches attributed to the TMJ and surrounding structures.
Trigeminal Neuralgia
Trigeminal Neuralgia is a chronic pain condition that involves pathological pain signaling from injury or compression of the trigeminal nerve. Symptoms include severe sensitivity to touch with even casual stimulation of nerve terminals in the face. Chewing and speaking can also trigger a pain response.
What type of doctor treats trigeminal neuralgia? This is an area of significant practice overlap, with practitioners including neurologists, neurosurgeons, ENT surgeons, and some dental specialists. The problem is that any one provider in these fields may or may not have training and expertise in treating trigeminal neuralgia. With the creation of the Orofacial Pain specialty, all orofacial pain practitioners are specifically trained to manage and treat trigeminal neuralgia patients. This includes medical pain management, the use of nerve blocks, and assessment to see if neurosurgical intervention is warranted, such as when there is vascular compression of the trigeminal nerve.
Orofacial Movement Disorders
Orofacial movement disorders affect the ability to control the muscles of the mouth, tongue, and jaw. Specific conditions include orofacial dyskinesia, orofacial dystonia, drug-induced movement conditions, and bruxism.
Orofacial dyskinesia and dystonia involve impairment of voluntary movement in the mouth, jaw, and tongue, usually in the form of repetitive or bizarre orofacial movements. Dyskinetic movements are more rapid, repetitive, and erratic, whereas dystonic movements are slow, protracted, and forceful. Orofacial Pain specialists are trained to treat orofacial dyskinesia and dystonia using Botox injections and other interventions.
Bruxism is defined as repetitive activation of the masticatory muscles that are either repetitive or sustained and is not attributable to an underlying movement disorder. Bruxism is classified as being either sleep bruxism or awake bruxism. Bruxism is usually not painful itself, but it is an independent risk factor for the development of TMJ pain. Orofacial Pain specialistsare trained to treat bruxism through a variety of means, including the directed use of intraoral devices (mouthguards specifically designed to address the type of bruxism.
Atypical Facial Pain
The term atypical face pain was developed to describe idiopathic face or teeth pain that did not fit into the typical patterns of trigeminal neuralgia or other orofacial pain disorders and is used as a diagnosis of exclusion. The pain can occur around the face or in the teeth and be episodic or chronic. It and is variably described as dull, aching, or burning pain distributed in a non-anatomic fashion in the teeth, gingiva, and other orofacial areas.
Orofacial pain specialists are uniquely qualified to treat atypical face pain because of its status as a diagnosis of exclusion. Unless one is trained to see the entire gamut of orofacial pain disorders, it is easy to misapply the category of atypical face pain to someone who has a defined disorder.
Burning Mouth Syndrome
Burning mouth syndrome is also called glossodynia, burning mouth syndrome consists of a burning sensation in the mouth or tongue without an obvious trigger. Symptoms can last for days to months or more. Xerostomia, dry mouth, and altered taste can also occur with burning mouth syndrome. Exacerbating factors include ingestion of alcohol, hot or spicy foods, and acidic foods. It affects women six times more frequently than men
Many practitioners, including primary care physicians and ENT doctors, may see isolated cases of burning mouth syndrome. Because it is so rare, these practitioners are typically unfamiliar with best practices for its treatment. In contrast, Orofacial Pain specialists are specifically trained in the diagnosis and treatment of burning mouth syndrome.
Relationship between Sleep Disorders and Orofacial Pain
Sleep disorders include sleep apnea, snoring, and sleep bruxism. There are many doctors who treat sleep apnea, including those trained in internal medicine, neurology, and orofacial pain. But why is orofacial pain on this list? The answer is three-fold.
First,
there is an increasing understanding that chronic pain and sleep disorders are linked. For instance, in the landmark OPPERA study on TMJ, patients with two or more indicators of sleep apnea had a 73% greater incidence of developing a TMJ disorder.
Second,
sleep apnea commonly presents with comorbid sleep bruxism. Per above, bruxism is classified as a movement disorder and is a risk factor for the development of TMJ disorders. Orofacial Pain specialists are qualified to treat this comorbidity using night guards and other interventions.
Third,
one of the main contributors to airway obstruction in sleep apnea is the tongue and jaw position. Because Orofacial Pain specialists are trained in dentistry, they are qualified to direct the fabrication and use of mandibular advancement devices (mouthguards calibrated based on the severity of obstructive sleep apnea present). They are also vigilant to see that such devices do not put the patient at risk for the development of TMJ disorders.
Orofacial Pain Specialists
Extensive training and clinical experience are required to become an Orofacial Pain specialist.
A licensed dentist must demonstrate years of exceptional understanding of the diagnosis and treatment of the various orofacial pain disorders. This is achieved by graduating from an advanced, university-based orofacial pain program that is CODA-accredited. These programs provide “education in orofacial pain at a level beyond predoctoral education relating to the basic mechanisms and the anatomic, physiologic, neurologic, musculoskeletal, vascular, behavioral and psychosocial aspects of orofacial pain.” In addition, to be certified, candidates must pass an examination administered by the American Board of Orofacial Pain (ABOP).
The rigorous post-doctoral training allows these specialists to accurately diagnose and treat both simple, complex, and multifactorial orofacial pain disorders. Without the knowledge and understanding attained by the training, both medical and dental clinicians may misdiagnose the problem, leading to inappropriate, and unsuccessful treatments. Sometimes unsuccessful treatment can lead to the incorrect conclusion that the patient’s pain is due to psychological factors.
Orofacial Pain specialists are expected to take primary responsibility for the coordination of care with a patient’s other healthcare providers. They must have an understanding of physical medicine, pharmacotherapeutic treatments, including systemic and topical medications and therapeutic injections, oral appliance therapy, non-surgical management of orofacial trauma, and behavioral therapies appropriate for treating patients with orofacial pain.
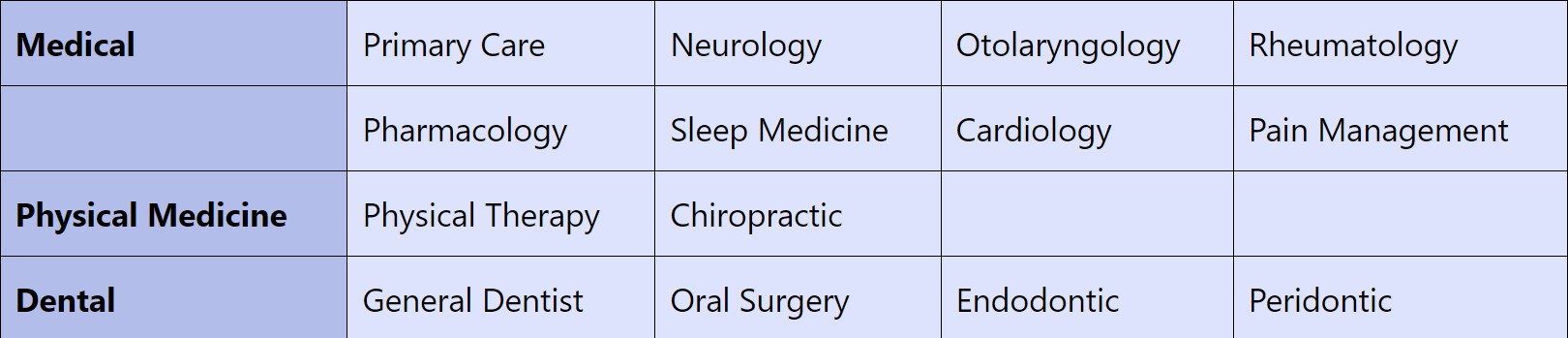
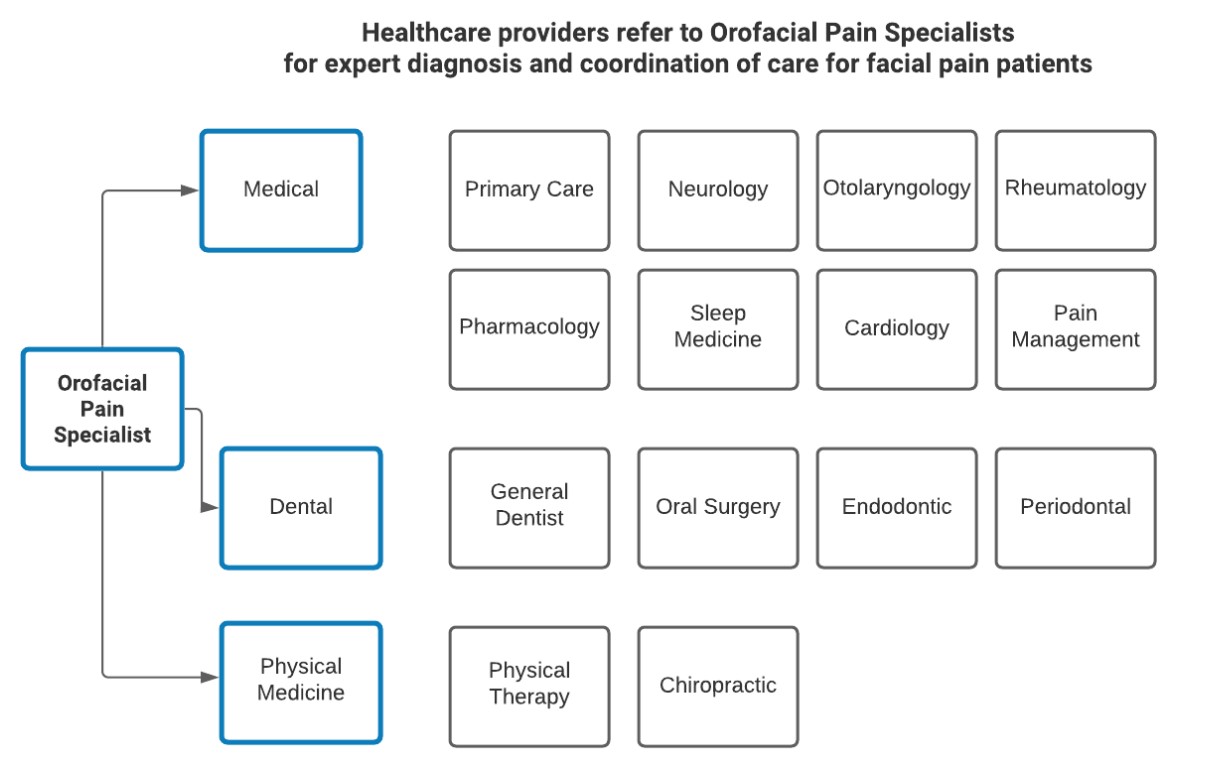
The chart below shows the extensive referral network to Orofacial Pain specialists from the medical, physical medicine, and dental communities.
These healthcare providers refer to Orofacial Pain Specialists for expert diagnosis and coordination of care for facial pain patients.
RESOURCES:
[1] American Academy of Orofacial Pain 2020 What is Orofacial Pain ?
[2] The Journal of the American Dental Association 2015.Orofacial pain, the 12th specialty


 Ask Prof. Hegab
Ask Prof. Hegab +201004401598
+201004401598

