If the flap / hood of gum (operculum) overlying a (wisdom) tooth becomes infected / inflamed, this elicits an operculitis, which is a form of pericoronitis.
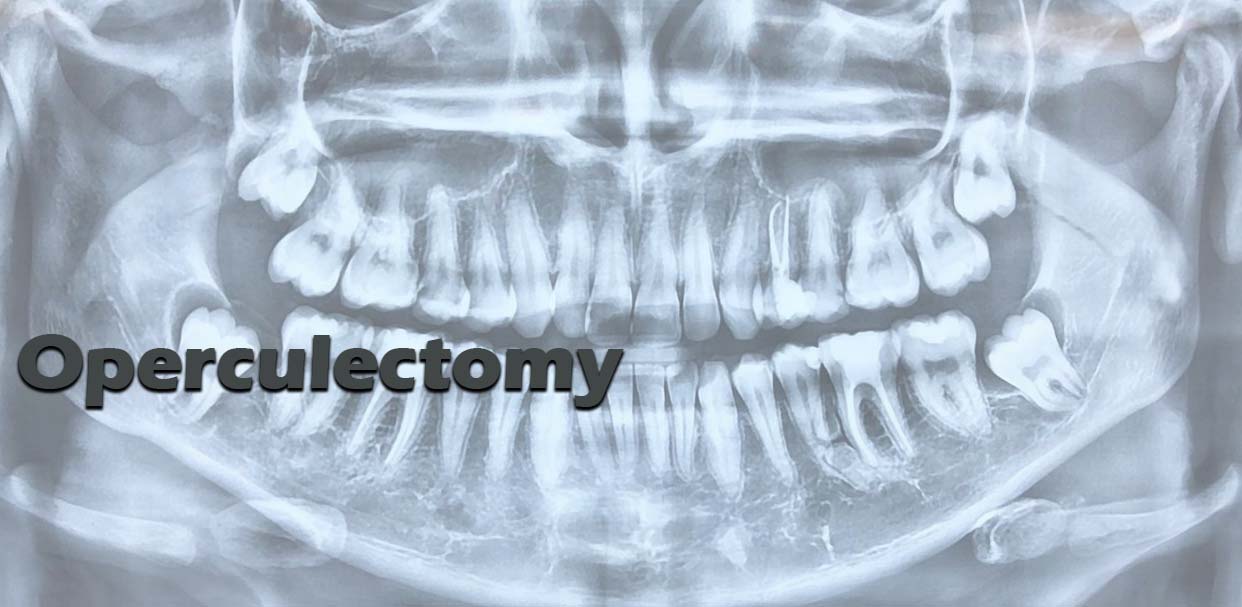
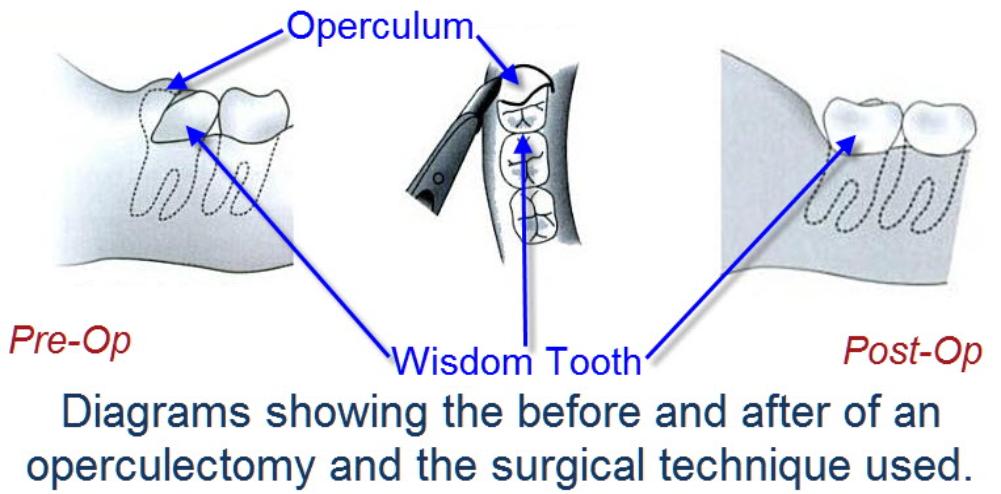
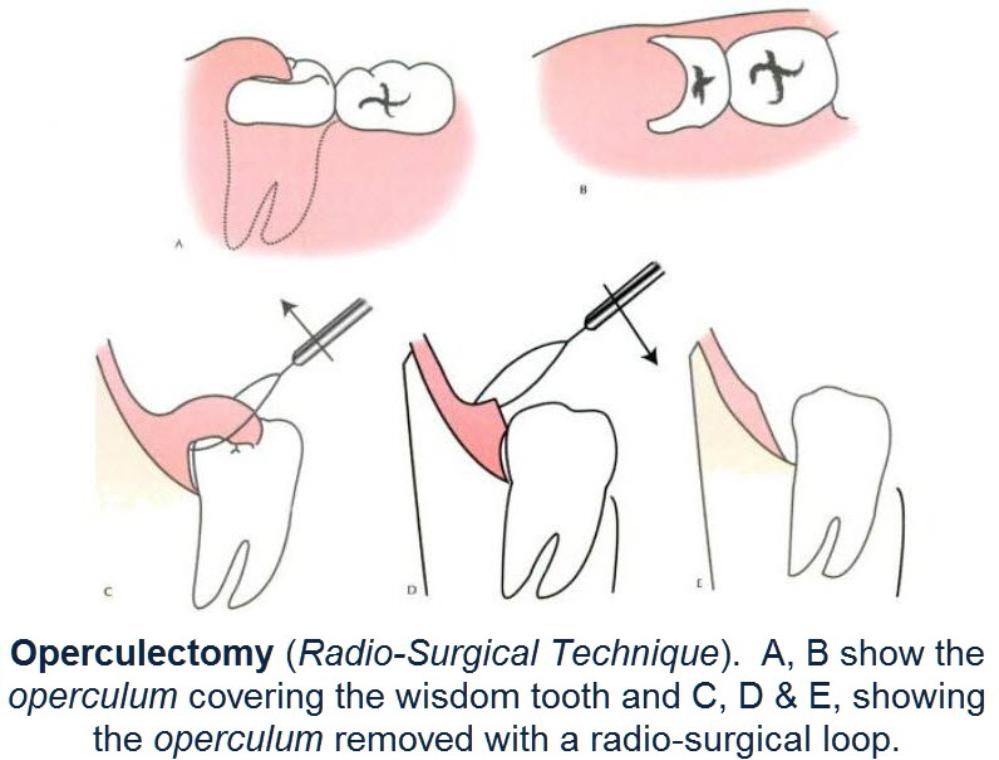
Operculectomy is the removal of the flap of gum overlying a tooth
Often, wisdom teeth are only partly erupted into the mouth. There is often a flap of gum (operculum) overlying the tooth. It is difficult to keep the area clean because of this flap. The flap can also be traumatised by the upper wisdom tooth biting onto it. If this is the case, the upper wisdom tooth may need to be removed as well.
Once the operculum has been removed, it should be easier to clean the area, lessening the risk of decay in the wisdom tooth (and the adjacent tooth) and of infection in and around the crown of the tooth.
The removal of the operculum can be achieved by a number of means (‘cold steel’, glacial acetic acid, radio-surgical means, laser or cautery).
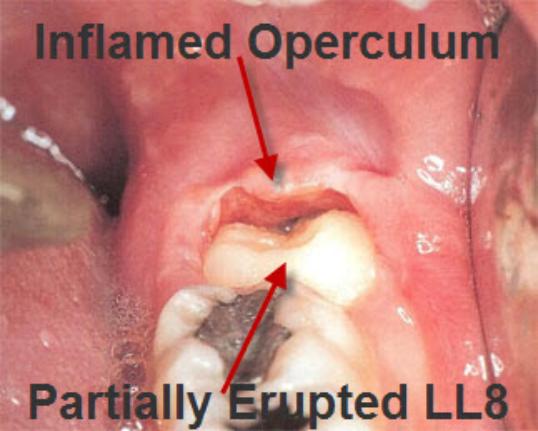

Photo of Pericoronits / Operculitis effecting Lower Jaw Wisdom Teeth
Problems with the procedure:
- It may not help at all.
- It possible that the operculum may grow back and the operculectomy may need to be repeated.
- The Lingual Nerve (supplies sensation to the tongue) may be effected. This can result in a numb tongue as well as loss of taste on that side of the tongue; the numbness can last up several months.
- If the wisdom teeth flare-ups have been quite episodic, then it may be hard to know if the operculectomy has in itself, been successful.
- The op site may become infected afterwards. This can happen in fit and healthy people with “clean mouths” and even if the patient is on antibiotics. Very occasionally, the infection may be such that the patient may need to be admitted to hospital for drainage of the abscess under a general anaesthetic.
An operculectomy is sometimes considered if the upper, opposing wisdom tooth is traumatising the operculum. The SIGN Guidelines suggest pain associated with the lower wisdom tooth is commonly exacerbated by the upper wisdom tooth biting on the gum flap (operculum), causing pain and discomfort.
Alternatively, if the upper wisdom tooth is easy to remove and is non-functional, then immediate removal of that tooth will often dramatically relieve the pain from the area. This is particularly useful where there is likely to be delay in the removal of the lower wisdom tooth and can be regarded as an interim measure (after referral but prior to surgery).
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
Operculectomy Specific Warnings:
Failure of Procedure. Even though an operculectomy may have been successfully carried out, there may still be problems of infection / inflammation around the crown of the tooth. That is, the operculectomy may not have worked.
Repeated Operation due to Regrowth of Operculum. The operculum can always grow back. If this is the case and the operculum is symptomatic, the operculum can be removed again. It is always possible that at this stage, the patient may just want to have the wisdom tooth removed.
Numbness of tongue ± loss of taste. The Lingual Nerve may be damaged during the procedure resulting in numbness (the “numbness” can range from “blunted sensation” to a burning sensation) affecting the tongue ± loss of taste to that side of the tongue. The numbness of the tongue ± loss of taste can last from weeks to months though it does have a low incidence.
Need to remove the upper wisdom tooth. The upper wisdom tooth may be biting on the operculum, traumatising it and exacerbating the painful symptoms. The patient may benefit from having this tooth removed as well.
Initial Appearance.
Initially, the operculectomy site may look somewhat disconcerting. It can appear raw, charred, deep, swollen and may bleed easily. The op site heals quite quickly (becoming noticeable after the 1st week or so). For the 1st week of healing, it is worth using an antiseptic mouthwash (such as Corsodyl or Peroxyl mouthwashes), a local an?sthetic mouthwash if painful (such as Difflam or Bongela) and hyaluronic acid gel / mouthwash (such as Gengigel).
General Surgical Warnings:
Pain.
As it is a surgical procedure, there will be soreness after the operculectomy. This can last for several days. Painkillers such as ibuprofen, paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history & the ease of the operation.
There will be swelling afterwards. This can last up to a week and peaks at around 2 – 3 days. Use of an icepack or a bag of frozen peas pressed against the cheek adjacent to the operation site will help to decrease the swelling. Avoidance in the first few hours post-operatively of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that will develop.
Bruising & Bleeding into Cheeks.
Some people are prone to bruise. Older people, people onaspirin or steroids will also bruise that much more easily. The bruising can look quite florid; this will eventually resolve but can take several weeks (in the worst cases).
Swelling that does not resolve within a few days may be due to bleeding into the cheek. The cheek swelling will feel quite firm. Coupled with this, there may be limitation to mouth opening and bruising. Both the swelling, bruising and mouth opening will resolve with time.
Stitches.
Where the operculum has been removed, it is often cauterised using electro-cautery, lasers, radio-frequency cautery or chemical cautery. These may need to be augmented with stitches. The stitches dissolve and ‘fall out’ within 10 – 14 days.
Limited Mouth Opening.
Often the chewing muscles and the jaw joints are sore after the procedure so that mouth opening can be limited for the next few days. If you are unlucky enough to develop an infection afterwards in the operation site, this can make the limited mouth opening worse and last for longer. There may also be scarring around the operation site – this scar can contribute to limited mouth opening.
Post-op Infection.
You may develop an infection in the operation site after the procedure. This though is rare. There may be swelling, limited mouth opening, pain, bad breath and an unpleasant taste in the mouth. If this happens, you need to contact your surgeon or dentist of A&E as soon as possible.
Occasionally, there may be a collection of pus from the infection that may need draining. This may be done under a general an?sthetic – if so, the wisdom tooth associated with the operculum may be removed at the same time.
Useful Articles & Websites
5- docdoc