Bruxism Treatment Strategies to Reduce Oral Parafunction
Tooth grinding behavior and temporomandibular joint pain: improving outcome through speedy treatment.
Oral parafunctional behavior is another name for teeth grinding. Oral parafunctional behavior (bruxism) is a movement disorder. Bruxism is the most recognized and studied type of oral motor behavior. Other behaviors include chewing gum, wind instrument playing, nail-biting and preferred chewing are other examples. This article provides tested bruxism treatment strategies that offer solutions for how to stop grinding teeth.
Self-Reporting Bruxism vs Clinical Measurement
There is an apparent association between oral parafunctional behavior (bruxism in particular) and painful temporomandibular disorders (TMDs). A recent review found that of 39 published studies examining the issue, 85% supported the existence of a positive association between bruxism and TMDs [1]. Despite these findings, there remains controversy regarding the extent and nature of this association.
First, there is often a discrepancy between self-reporting and visual or clinical proof of its presence. A series of studies compared the self-reporting of sleep bruxism with sleep bruxism as documented by Polysomnography. Although there was a statistically significant association between self-reported bruxism and painful TMD symptoms, this association disappeared when comparing instrument-defined bruxism and painful TMDs.
Considerations in explanation for this discrepancy is self-reporting affected by patient bias resulting in an overestimation of prevalence. Other explanations are that sleep bruxism may be daytime behavior that is assumed to be present or continued during sleep. Several studies show that a self-report of both sleep and awake bruxism is significantly more predictive of TMD pain than a report of either alone [2].
Also, because both conditions are present in 10% of the population, it is difficult to define the relationship based solely on population study.
Orofacial Pain: Prospective Evaluation and Risk Assessment (OPPERA) Study
An NIH prospective study report by Richard Ohrbach et al.; examines the factors that precipitate and maintain TMD pain. The Clinical Findings and Pain Symptoms as Potential Risk Factors for Chronic TMD: Descriptive Data and Empirically Identified Domains from the OPPERA Case-Control Study offers unique insight into the issue. The OPPERA study found that “where parafunctional behaviors were assessed on a continuum using a comprehensive questionnaire, odds of TMD was elevated 17-fold among people in the upper tertile of the distribution relative to people in the lowest tertile”.
This is a significant finding given in the November 12, 2011 report that helps orofacial pain specialists. It is a longitudinal study and thus not subject to the same issues as other population studies.
Oral parafunctional behavior when muscle pain and clenching are mutually reinforcing.
Importantly, the OPPERA researchers suggest that based on the magnitude of the association, there is likely a bidirectional rather than causal relationship between oral parafunctions and painful TMDs. Said another way, the OPPERA study infers that in certain cases, a mutually reinforcing relationship between pain and oral parafunction exists. The fact that people with masticatory muscle pain display an increased frequency of high and low-intensity daytime clenching is supportive of the idea that muscle pain and clenching are mutually reinforcing [3].
The association of oral parafunction and chronic pain open treatment opportunity for early intervention and reduction of TMD. Parafunctional behavior treated promptly may prevent the development or reverse the risks of more chronic jaw conditions.
Here we cover the physiological principles that connect parafunctional behaviors and chronic TMD pain, the clinical aspects of oral parafunctions and where intervention might be most appropriate, and the conservative therapeutic interventions that can be made to prevent chronic pain.
Oral parafunctions such as bruxism are multifactorial in origin and are not fully understood. One constant, however, is parafunctional behavior represents tonic or repetitive contraction of facial muscles. Prolonged masticatory muscle activation is sufficient to manifest trigger TMD pain symptoms in normal patients and is positively associated with the intensity of masseter muscle activity.
Here we focus mainly on the association of bruxism and muscle-related TMD, recognizing bruxism is the most common form of parafunction behavior with a strong association with a muscle-based disorder.
Even minor bruxing and clenching is enough to trigger TMD pain. One study evaluated low-level elevations in masseter EMG recordings, those that were higher than baseline levels but below consensus criteria for bruxism. The results showed a significant association between these small, persistent elevations in EMG activity and patient reports of painful TMD symptoms.
A recent meta-analysis finds the activity of the masticatory and temporalis muscles are significantly higher at risk in patients suffering from TMDs [4]. Elevations of EMG recordings contribute to painful TMDs. They may represent low-energy muscle contractions adding to the induction or maintenance of TMD pain.
The Efficacy of Hegab Splint Therapy for Painful TMDs
With early diagnosis, bruxism treatment strategies that include Hegab splint (mouthguard) therapy have proven efficacy.
Inhibiting oral parafunctional behavior provides relief from painful TMD symptoms. Many studies claim that the efficacy of Hegab splint therapy for painful TMD is directly related to their ability to decrease oral parafunctional behavior. However, several studies have shown that paralysis of the masseter muscle with botulism toxin provides a significant decrease in TMD pain symptoms [5].
Reducing one part of a complex relationship between bruxism and TMD pain can assist in the interruption of the overall pain cycle. Within local tissue, bruxism is associated with chronic muscular contraction which causes tissue hypoxia. This in contrast to low-energy, long-duration clenching is currently a topic of research. Various inflammatory mediators and cytokines along with the inflammatory sensation of peripheral neurons can result in peripheral sensitization.
How does peripheral sensitization impact chronic pain syndromes?
Peripheral sensitization occurs in the afferent nerves of the TMJ complex when the threshold response of these nerves is lowered through repetitive response. This leads to a state of increased reactivity to painful stimuli, called “hyperalgesic priming.” Hyperalgesic priming is mediated by pro-inflammatory cytokines that are released with tissue ischemia, such as prostaglandins.
Peripheral sensitization can lead to central sensitization. This phenomenon is the neurophysiological hallmark of chronic pain syndromes. Central sensitization describes a neuroplastic change within the central nervous system where pain circuits become hyperexcitable. These are confirmed on examination with findings including allodynia, hyperalgesia, and secondary hyperalgesia. This process occurs over days to weeks and involves increased expression of pro-inflammatory cytokines, morphological changes in microglial and other supporting cells, and changes in central and peripheral synaptic connectivity [6].
What is the Relationship between Anxiety Symptoms and Bruxism?
Psychological factors also influence the pathophysiological association between oral parafunctions and painful TMDs. The amygdala is the site of affective states such as anxiety and depression. In chronic pain, there are neuroplastic changes in the so-called “nociceptive amygdala” that amplify pain signals, contributing to the clinical findings of allodynia and hyperalgesia. This is important in this context because of the strong relationship between anxiety symptoms and bruxism.
It’s important to note here that while oral parafunction, psychological stress, and chronic pain may co-exist, they are not necessarily causality related.
Multiple studies lead to largely consistent findings: stressful states can trigger parafunctional episodes that contribute to myofascial pain. However, this simple causal pathway coexists with at least 3 other pathways: anxiety and stress are potent direct contributors to pain, pain results in maladaptive behaviors such as parafunction, and parafunction may be a coping response to potential threat coupled with hypervigilance and somatosensory amplification.” – Ohrbach and colleagues (2018) [7]
Therefore, oral parafunction and psychosocial factors do not necessarily cause chronic TMDs. Many attributing factors remain both known and yet be identified that contribute to TMD chronicity.
What is the difference between bruxism and TMD disorder?
Bruxism may be caused by TMD; however, bruxism can in turn also trigger or worsen TMD. Untreated bruxism-related muscle pain has the potential to decrease jaw mobility and thus may result in a persons’ protective response. Intense concentration or situational anxiety (which is not an anxiety disorder), may cause a person to clench or grind their teeth unconsciously. A TMD disorder may be avoided if they become aware of their teeth grinding habit and their jaw muscle tension can ease and normalize.
According to John Hopkins Hospital, “Bruxism (jaw clenching or teeth grinding) can make a TMJ disorder more likely. It overworks the TMJ, which can lead to a disc in the joint wearing down or move out of place. Grinding and clenching also can change the alignment of the bite (the way that top and bottom teeth line up) and can affect the muscles used for chewing”.
Regular dental professionals value the insights of orofacial pain specialists who understand the relationships between teeth clenching or grinding and a possible temporomandibular joint disorder. They assist with creating mouth and jaw pain coping strategies by also assessing possible correlated symptoms like mental health trauma or sleep apnea triggers.
Likewise, a patient who gains a clear diagnosis and treatment plan can feel more confident of being on the path to recovery. Frequent bruxers’ ability to visualize a positive outcome and maintain good coping skills during treatment has an important role as a causative factor. We find that patients who embrace positive coping strategies report reduced jaw tension and a higher level of well-being.
Patients with Both Bruxism and TMD Symptoms: Clinical Considerations
Patients who manifest both bruxism and painful TMD symptoms will be considered. Early intervention with conservative measures can be used to interrupt the transition from acute to chronic TMJ pain. Additionally, it helps to address the pain cycle of those who already have painful TMDs.
A clinical history can reveal the patients with oral parafunctions who are more likely to develop chronic TMD
How Does Simple Patient Self-reporting Improve Outcomes?
Two suggested questions in the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/ TMD) for self-reporting bruxism are:
- “Have you been told, or do you notice that you grind your teeth or clench your jaw while sleeping at night?”
- “During the day, do you grind your teeth or clench your jaw?”
If the jaw injury self-report is positive for bruxism, a more comprehensive evaluation for oral parafunctional behaviors can be performed. One tool for this is the Oral Behavioral Checklist (OBC), a 21-item questionnaire that surveys a range of oral behaviors beyond bruxism. Recall that the OPPERA study found a 17-fold increase in TMD incidence in those in the top tercile of OBC scores [6].
Practitioners should evaluate for any psychosocial features that are known to contribute to TMD development. These include screening for general medical status, overall pain status, somatization, depression, and anxiety. Standardized and validated questionaries for these risk factors are outlined in the Axis II component of the RDC/TMD. Psychosocial evaluation is critical because, in the OPPERA study, features such as somatization, stress, and emotional distress were predictive of the first onset of TMDs.
How do Orofacial Pain Specialist Assess Bruxism?
The physical examination for bruxism can also establish the presence of oral parafunctional behavior and determine the best bruxism treatment strategies.
Here are some common findings to look for during the assessment of bruxism:
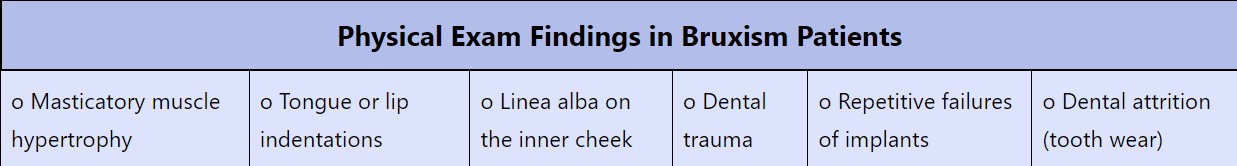
When physical signs are weak or absent, the possibility of bruxism is not eliminated. A recent study evaluated the accuracy of tooth wear for diagnosing bruxism using a polysomnogram as the gold standard test. Researchers found that as a diagnostic test for bruxism, dental attrition has only a 30% sensitivity [8].
What are Current Bruxism Treatment Strategies?
Interruption of oral parafunction is the most supported method to prevent the development of a chronic TMD state. Similarly, an established chronic TMD may also be addressed using a similar treatment and provides substantial symptomatic relief.
Treating bruxism is actually a process, a neuromuscular treatment process using non-invasive and effective solutions.
We have established that while there is no direct causality between oral parafunction and TMD development, there is a reticulum of influence between the two. We contend that by interrupting the influence of the former, we might be able to prevent the development of a chronic painful TMD state. Similarly, an established chronic TMD may also be addressed using similar treatment and provides substantial symptomatic relief.
Treatment of painful bruxism with botulism toxin (Botox) is an excellent illustration of this point. Recent meta-analysis evaluating Botox for the treatment of bruxism found that Botox is effective in reducing pain and jaw stiffness. On the other hand, Botox did not decrease the number of bruxism episodes as documented by polysomnogram [9].
How do Hegab Splints Offer Treatment for Bruxism?
Hegabl splints offer an equal opportunity to treat bruxism. Hegab splints decrease the level of movement, provide a non-chemical myorelaxant effect, and have been shown to decrease pain. Additionally, Hegab splints are reliably effective in established TMD patients. These findings indicate that Hegab splint therapy can be instrumental in the treatment of painful oral parafunction and preventing TMD chronicity.
A splint is designed to provide relief from pain and improvement jaw function so it moves smoothly. The splint is useful to many patients as the first step in a multi-step procedure. This form of conservative bruxism treatment may produce changes in the bite and in jaw positions, which are reversible if needed.
Hegab Splint Therapy and Other Conservative Interventions
Rather than using any one intervention on its own, we believe a multimodal strategy is optimal for interrupting the conditions that establish chronic pain. In addition to Hegab splint therapy, we recommend using the following.
Conservative interventions that have shown to be effective in reducing TMD symptoms:
- Cryotherapy: Cold causes vasoconstriction, reduces inflammation, reduces pain, and decreases jaw muscle tension.
- Thermotherapy: Heat causes vasodilation, increases tissue oxygenation, facilitates waste elimination, promotes muscle relaxation, and increases mobility.
- Physical Therapy: Mobility circulates synovial fluid, removes metabolic waste, and interrupts peripheral sensitization. Jaw pain patients consistently report that physical therapy is effective in their TMD treatment.
- Behavioral Pain Management: Behavioral therapy teaches resilience to anxiety and stress from pain. Behavioral therapy also addresses the psychological aspects of chronic pain.
Supporting the self-management of chronic pain conditions with self-assessments.
Finally, it’s important to note that the above conservative interventions are consistent with a patient-directed therapy approach. Self-management is a keystone element in the management of chronic pain conditions such as TMDs [7]. Patients who believe themselves capable of proactively changing the course of their disease have better outcomes. A 2010 study by Van der Meulen evaluating illness beliefs of TMD patients with bruxism, 90% believed their parafunction could be reduced and 92.% believed they were capable of doing so. This demonstrates the power of symptom management and self-regulation.
Efficiency of Occlusal Splint Therapy.
Orofacial Therapeutics’ review of management strategies for bruxism after consideration of later published randomized controlled trials concludes that the positive effect of oral appliances on bruxism is best with early treatment, variable, and can be challenging to interpret. More positive studies supporting the efficiency of occlusal splint therapy will help in reducing the negative consequences of bruxism and reinforce conservative bruxism treatment modalities.
Some oral parafunctional behaviors and painful TMD symptoms are clearly associated. As with many disorders, prompt treatment with conservative measures – including belief – are powerful tools to interrupt the relationship between oral parafunction and TMJ pain. We have shown early intervention to be the most useful intervention in the development of TMD chronicity.
Bruxism (teeth grinding) Diagnosis and Treatment Conclusion
Using simple screening tests, a clinical profile of individuals vulnerable to TMD development due to teeth grinding issues can be detected. We recommend these patients should be offered an early bruxing intervention strategy focused on preventative treatment which is conservative, patient-directed, and comprehensive.
The multimodal approach should be directed at the pain symptoms and not limit its impact on the decrease of oral parafunctional behavior alone. This early intervention can interrupt the neurological processes which are shown to place patients at risk of chronic TMD pain.
References
1. Jiménez-Silva, et al. Sleep and awake bruxism in adults and its relationship with temporomandibular disorders: A systematic review from 2003 to 2014. Acta Odontologica Scandinavica, https://doi.org/10.1080/00016357.2016.1247465 (2017)
2. Berger, M., et al. Different association between specific manifestations of bruxism and temporomandibular disorder pain. https://doi.org/10.1016/j.pjnns.2016.08.008 (2017)
3. Cioffi, et al. Frequency of daytime tooth clenching episodes in individuals affected by masticatory muscle pain and pain-free controls during standardized ability tasks. https://doi.org/10.1007/s00784-016-1870-8 (2017)
4. Dinsdale, A., et al. Is jaw muscle activity impaired in adults with persistent temporomandibular disorders? A systematic review and meta-analysis. Journal of Oral Rehabilitation, https://doi.org/10.1111/joor.13139 (2021)
5. Kaya, D. I., & Ataoglu, H. Botulinum toxin treatment of temporomandibular joint pain in patients with bruxism: A prospective and randomized clinical study. https://doi.org/10.4103/njcp.njcp_251_20 (2021)
6. National Academies of Sciences. Introduction. In Temporomandibular Disorders: Priorities for Research and Care. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK557989/ (2020)
7. Ohrbach, R., & Michelotti, A. (2018). The Role of Stress in the Etiology of Oral Parafunction and Myofascial Pain. Oral and Maxillofacial Surgery Clinics of North America, https://doi.org/10.1016/j.coms.2018.04.011
8. Palinkas, M., et al. Comparative Capabilities of Clinical Assessment, Diagnostic Criteria, and Polysomnography in Detecting Sleep Bruxism. Journal of Clinical Sleep Medicine : JCSM : Official Publication of the American Academy of Sleep Medicine. https://doi.org/10.5664/jcsm.5196 (2015)
9. De la Torre Canales, et al. Is there enough evidence to use botulinum toxin injections for bruxism management? A systematic literature review. Clinical Oral Investigations, https://doi.org/10.1007/s00784-017-2092-4 (2017)