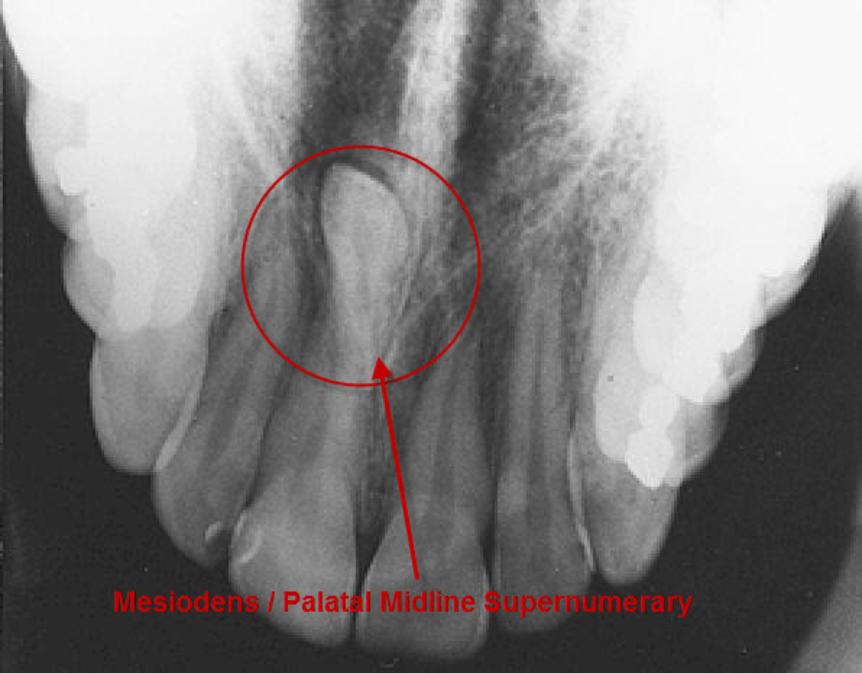
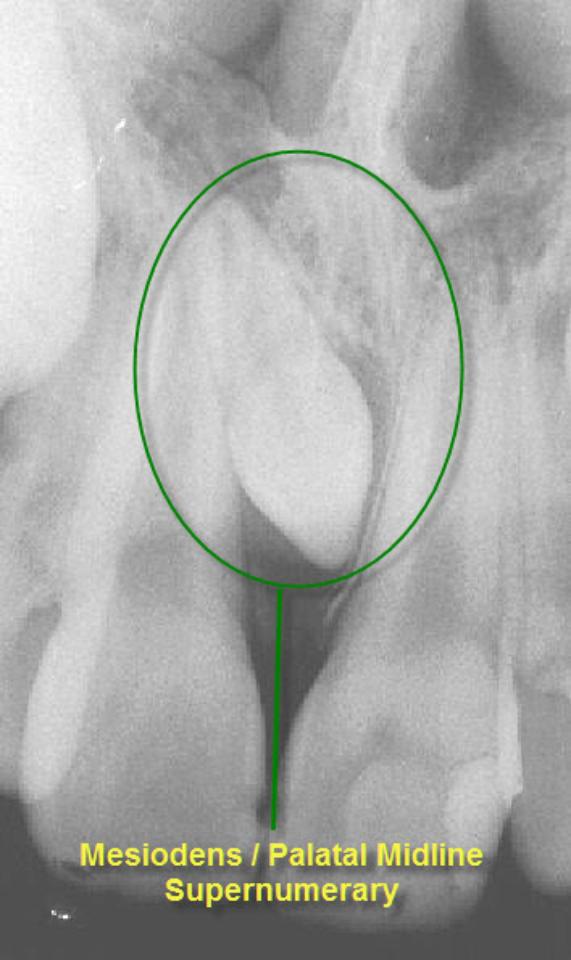
It is quite common to have extra teeth (supernumerary teeth) or teeth in the wrong position (ectopic teeth) or both.
The prevalence of supernumerary teeth is reportedly between 0.15 – 3.9%. Most commonly, extra teeth are found between the upper central incisors (mesiodentes) or in the region of the premolars (paramolars) or very occasionally, behind the wisdom teeth (distomolars).
Supernumerary Teeth.
80 – 90% of all supernumerary teeth occur in the upper jaw. Half are found at the ‘front’ of the upper jaw. Mesiodentes frequently interfere with the eruption and alignment of the upper incisors. They can delay or prevent eruption, displace or rotate the erupting central incisors or less commonly, ‘bend’ (dilaceration) the developing roots of the central incisors so that tooth eruption is slowed / stopped, ‘eat away’ (resorption) the surrounding teeth, develop cysts around the crowns of the extra teeth (dentigerous cyst formation) and loss of tooth vitality. Rarely, the mesiodens can erupt into the nasal cavity
Ectopic Teeth.
Ectopic teeth are teeth that develop in the wrong position. Ectopic teeth are not rare. In most cases, ectopic tooth can be repositioned with braces.

The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
Ectopic ± Supernumerary Surgery-Specific Warnings.
Numbness of the Lip, Chin ±Tongue.
The nerves that supplies feeling to the tongue, lower lip and the chin run risk that when bicuspid teeth squeezed out of the line of teeth towards the tongue are removed, these nerves can be crushed, bruised or stretched resulting in numbness (at the worse end of the scale) to altered sensation (at the other end of the scale) in the region of the lower lip, chin and/or tongue. This nerve bruising tends to be temporary (rarely is it permanent) but ‘temporary’ can stretch from several days to several months. It is hard to predict who will get nerve bruising and if it will be temporary / permanent and if temporary, how long for.
Mouth-Sinus Communications.
Upper premolar & canines are often in close proximity to the sinus. In removing these teeth, there is a chance that a communication can be made between the mouth & the sinus (this is sometimes not evident at the time of operation but may develop 4 – 6 weeks afterwards). If this communication persists or is left un-repaired, every time you drink, fluid can come out of the nose and you may develop a marked sinusitis. This communication, if small enough, can spontaneously close. It can be assisted in this by ‘cover plates’ that prevent food & fluids going into the sinus allowing the hole to close naturally. However, communications above a certain size need to be surgically closed.
Surrounding Teeth.
The surrounding teeth may be sore after the extraction; they may even be slightly wobbly but the teeth should settle down with time. It is possible that the fillings or crowns of the surrounding teeth may come out, fracture or become loose. If this is the case you will need to go back to your dentist to have these sorted out. Every effort will be made to make sure this doesn’t happen.
In very rare instances, the surrounding teeth may actually come out as well as the intended tooth (tooth avulsion). Extra teeth can be very hard to get at and in doing so, the blood-supply to the surrounding teeth may be compromised. If this happens, these teeth can die (under go ‘devitalisation’); the teeth change colour (turn grey), become spontaneously painful or become infected. A tooth that is dying may not be immediately obvious and may take several weeks to become so.
General Surgical Warnings.
Pain.
As it is a surgical procedure, there will be soreness after the tooth removal. This can last for several days. Painkillers such as ibuprofen, paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history & the ease with which the tooth was removed.
Swelling.
There will be swelling afterwards. This can last up to a week. Use of an icepack or a bag of frozen peas pressed against the cheek adjacent to the tooth removed will help to decrease the swelling. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that will develop
Occasionally, there is bleeding into the cheek. The swelling caused by this may take much longer to resolve; at the same time, there may well be limitations to mouth opening. This also improves with time.
Bruising.
Some people are prone to bruise. The bruising can look quite florid; this will eventually resolve but can take several weeks (in the worst cases).
Stitches.
The operation site will often be closed with stitches. These dissolve and ‘fall out’ within 10 – 14 days.
Limited Mouth Opening.
Often the chewing muscles and the jaw joints are sore after the procedure so that mouth opening can be limited for the next few days. If you are unlucky enough to develop an infection in operation site afterwards, this can make the limited mouth opening worse and last for longer.
Bleeding into Cheeks.
Swelling that does not resolve within a few days may be due to bleeding into the cheek. The cheek swelling will feel quite firm. Coupled with this, there may be limitation to mouth opening and bruising. Both the swelling, bruising and mouth opening will resolve with time.
Post-op Infection.
You may develop an infection in the socket after the operation. This tends to occur 2 – 4 days later and is characterised by a deep-seated throbbing pain, bad breath and an unpleasant taste in the mouth. This infection is more likely to occur if you are a smoker, or are on the contraceptive pill, or on drugs such as steroids and if bone has to be removed to facilitate tooth extraction.
Surgical Removal.
To facilitate the removal of teeth, it is sometimes necessary to cut the gum and / or remove bone from around the tooth. If this is the case, you can expect the extraction site to be sorer afterwards, the swelling to be greater and more prone to infection. Hence, stronger painkillers are needed; use of icepacks mandatory and antibiotics will probably be prescribed. The bone grows back to a greater extent.
Bony Flakes.
If a number of teeth are removed at one go, the resulting gums may feel a bit rough. Occasionally, bony flakes (sequestra) from the lining of the tooth sockets can work their way loose out through the gums. These can be quite sore. They often work their way loose without any problems but may need to be teased out or even smoothed.
Useful Articles & Websites
1- Australian Dental Journal 1998. Supernumerary tooth in the maxillary sinus. Case report
6- New England J of Medicine 2011. Images in Clinical Medicine. Ectopic Tooth in the Maxillary Sinus
8- Wikipedia