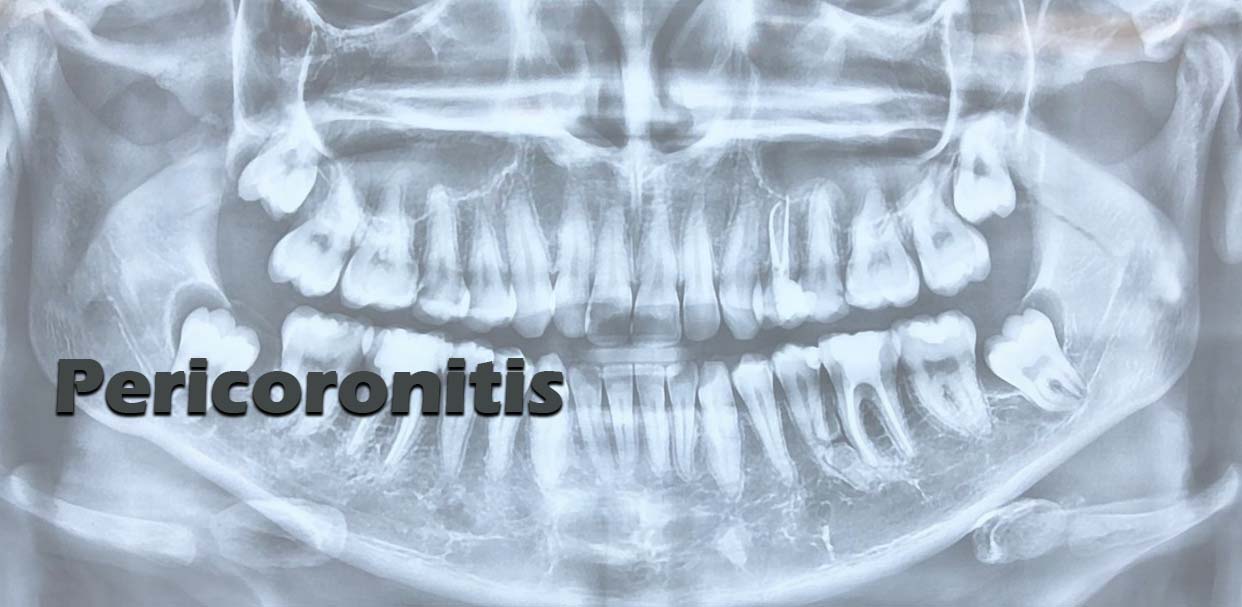
Pericoronitis is inflammation in the soft tissues (such as the gingiva and dental follicle) surrounding the crown of a partially erupted tooth, usually the lower 3rd molar (wisdom tooth).
It generally does not arise in teeth that erupt normally; usually, it is seen in teeth that erupt very slowly or become impacted and it most commonly affects the lower 3rd molar.
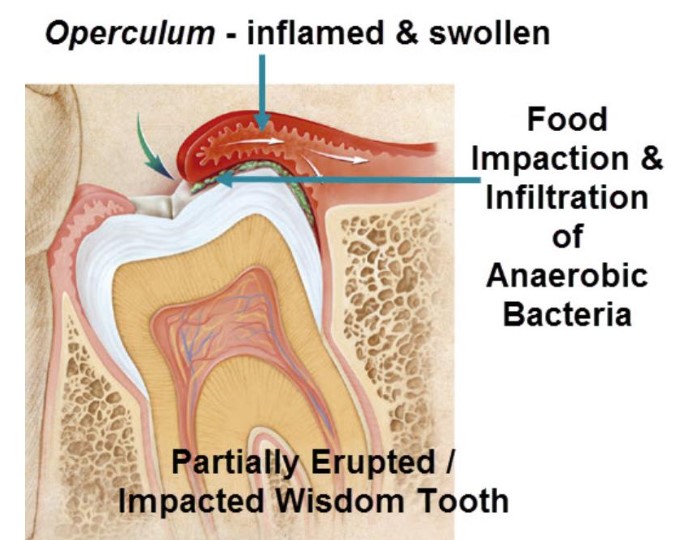
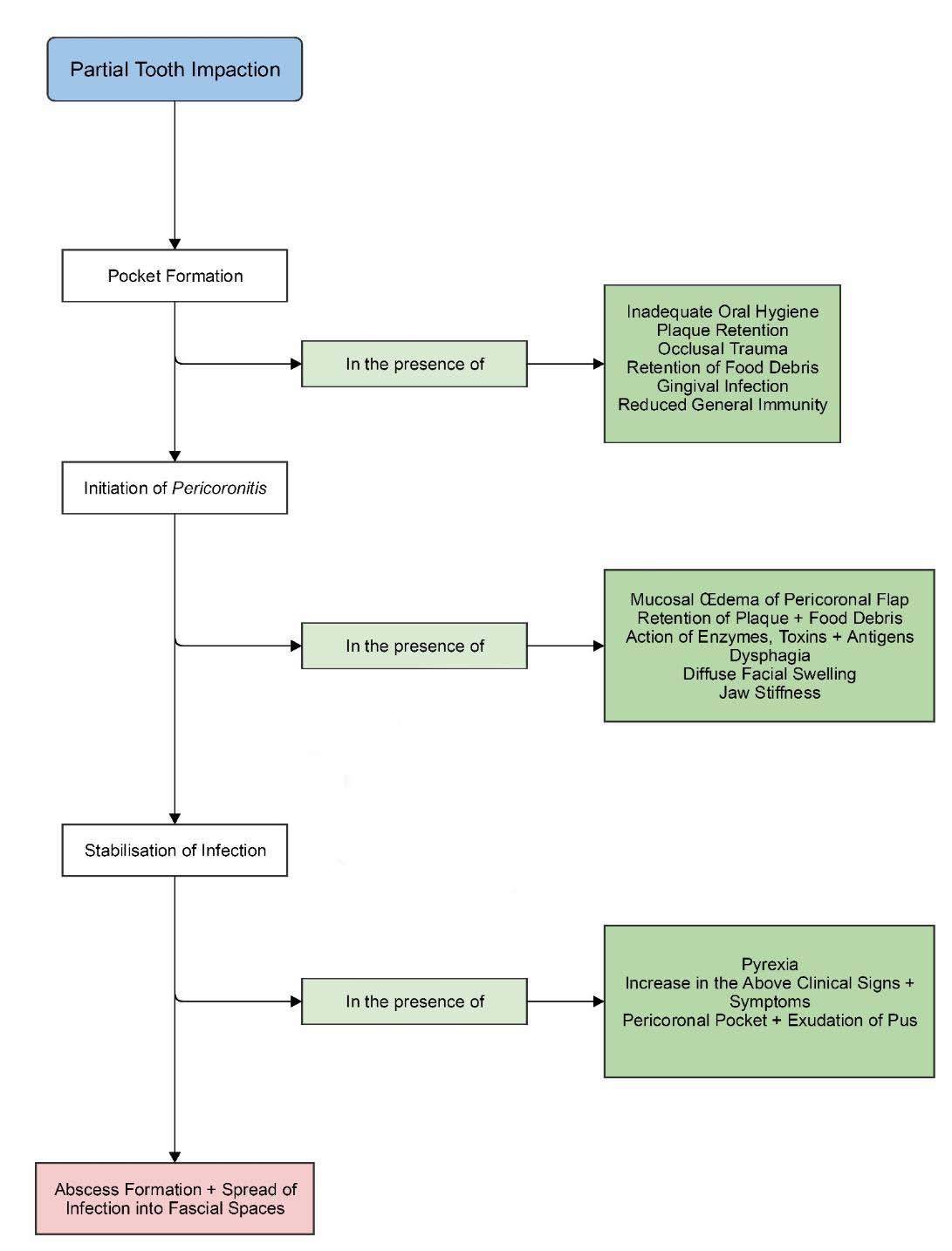
Once the follicle of the tooth communicates with the oral cavity, it is thought that bacterial infiltration into the follicular space initiates the infection.
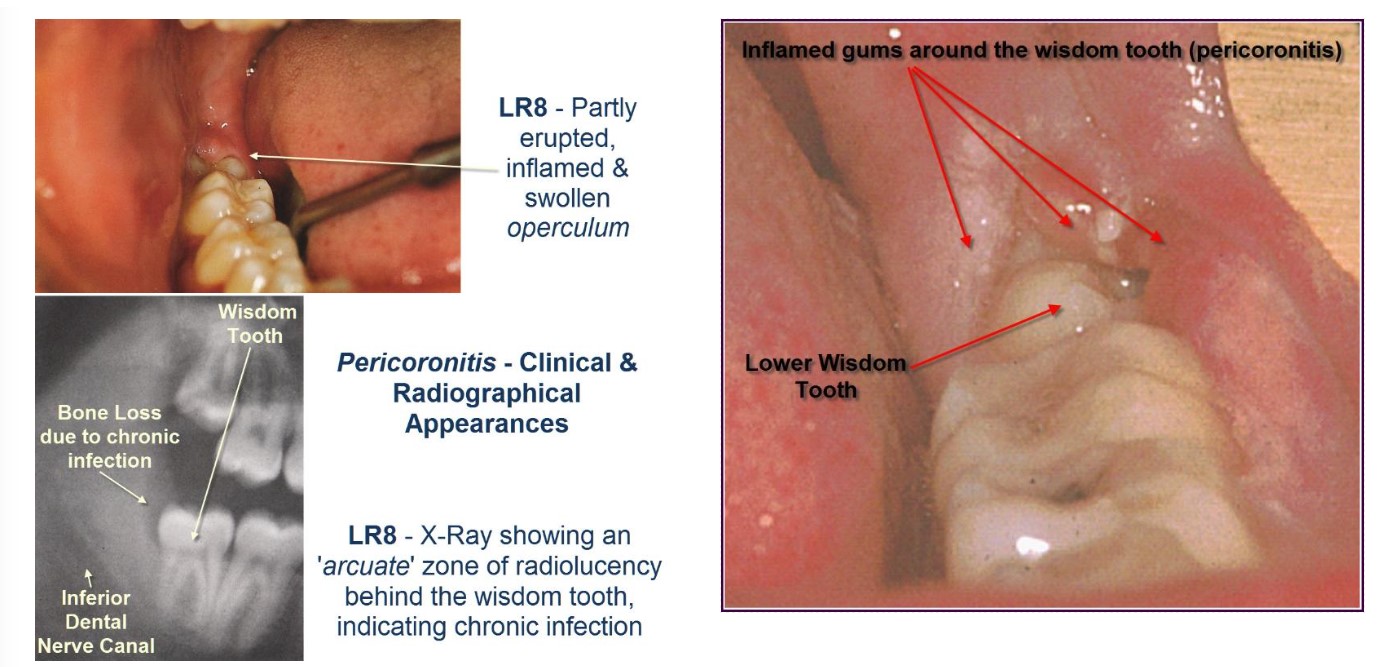
The soft tissue covering over a partially erupted tooth is known as peri-coronal flap or gingival operculum. Maintenance of oral hygiene in such area can be very difficult to achieve by normal methods of oral hygiene.
There was no significant difference between the sexes.
A seasonal variation is noted with peak incidences occurring in June and December.
Bilateral (both sides) pericoronitis is rare and suggests underlying infectious mononucleosis (Glandular Fever).
Acute:
Acute pericoronitis is of sudden onset, short lived but having significant symptoms, such as varying degrees of inflammatory involvement of the pericoronal flap. There is also a presence of systemic involvement. Usually, the acute form of pericoronitis is seen in the patients having poor oral hygiene.
Acute Pericoronitis – Clinical Features:
- Caused 2nd to occlusal trauma from maxillary (upper) 3rd molar on retro-molar region (area behind the lower wisdom tooth)
- Operculitis (Inflammation of the operculum).
- Severe redness + soreness
- Continuous severe pain
- Localised intra-oral swelling
- Trismus (limited mouth opening)
- Foetor ex ora (bad breath)
- Lymphadenitis ++
- Malaise
- Leucocytosis
- Dysphagia (problems eating)
- Pyrexia (fever) associated with tachycardia (increased heart rate) if neglected
Sub-Acute Phase of Pericoronitis – Clinical Features:
- Intra- & Extra-oral swelling
- Severe trismus
- Pyrexia & malaise
- foetor ex ora
- Severe pain in retro-molar region
- Inflammation of masticatory muscles (chewing muscles)
- Dysphagia, pyrexia & tachycardia are severe
- Operculum ulceration
- Lymphadenitis +++
- Peri-coronal pus ++
- Fascial space infections of neck & mandible (Ludwig’s Angina, Para-pharyngeal abscess)
Chronic:
Pericoronitis may also be classified as chronic / recurrent. Acute pericoronitis occur repeatedly and periodically. It may cause few symptoms but some signs are visible at the time of intra-oral examination. The chronic type mostly seen with good-moderate oral hygiene.
The main complaint is of a dull pain or mild discomfort lasting a day or two, with remission lasting many months. Cacogeusia (bad taste) may also be present. Pregnancy and fatigue are associated with an increased occurrence of pericoronitis.
Chronic Pericoronitis – Clinical Features:
- Localised tissue swelling & redness
- Soreness
- Continuous dull pain
- Localised rise in temperature
- Lymphadenitis +
The most common site of pericoronitis is impacted or partially erupted lower 3rd molar.
The most common cause behind peri-coronal inflammation is the entrapment of plaque and food debris between tooth crown and overlying operculum (gum flap). This is an ideal area for the growth of bacteria and it is difficult to keep clean; also, there is the constant possibility of acute inflammation of peri-coronal (around the crown of the tooth) sites. It may be due to trauma, occlusion or entrapment of foreign body below the peri-coronal flap / operculum.
Risk Factors:
- Presence of unerupted / partially erupted tooth / teeth in communication with the oral cavity. Lower 3rd molars (which are vertically and disto-angularly impacted) are most commonly affected
- Presence of periodontal pocket adjacent to unerupted / partially erupted teeth
- Opposing tooth / teeth in relation to peri-coronal tissues surrounding unerupted / partially erupted tooth / teeth
- Previous history of pericoronitis
- Poor oral hygiene
- Respiratory tract infections & tonsillitis
- Age (20 – 29 year age group; the condition was rarely seen before 20 or after 40).
- Emotional stress
Management:
These include debridement of plaque and food debris, drainage of pus, irrigation with sterile saline, chlorhexidine or hydrogen peroxide & elimination of occlusal trauma.
In the past the use of caustic agents such as chromic acid, phenol liquefactum, glacial trichloroacetic acid or Howe’s ammoniacal solution was advocated to control pain by placing a small amount on a cotton pledget under the operculum.
The resultant chemical cauterisation of the pain nerve endings in the superficial tissues gave rapid pain relief; however, the use of these toxic chemicals in the oral cavity is no longer encouraged.
Ozone has been put forward as a local antimicrobial that might be a useful adjunct in the treatment of pericoronitis; however, there is no research available to show its efficacy as yet.
In addition to local pain and swelling, if the patient is exhibiting regional or systemic signs and symptoms, antimicrobial therapy (such as metronidazole) is recommended; however, it should be emphasised that it is as an adjunct rather than a 1st line treatment. These are all active against an?robic bacteria, which are the predominant microflora found in pericoronitis.
Once the acute phase of the pericoronitis has passed, operculectomy has been used as a preventive measure.
Useful Articles & Websites
J Ir Dent Assoc 2009. Pericoronitis – A Treatment & A Clinical Dilemma