Typically, the tooth is extensively decayed or fractured and is causing chronic infection and discomfort.
Sometimes, the tooth has to be removed surgically. Surgical removal is needed when simple extraction is not possible because of the condition of the tooth.
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
The following list of warnings regarding tooth extraction is neither exhaustive nor is it predictive. The most pertinent warnings have been included here.

Indications for Tooth Removal
Common Surgical Consequences:
Pain.
As it is a surgical procedure, there will be soreness after the tooth removal. This can last for several days. Painkillers such as Ibuprofen, Paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history & the ease with which the tooth was removed
Swelling.
There will be swelling afterwards. This can last up to a week. Use of an ice-pack or a bag of frozen peas pressed against the cheek adjacent to the tooth removed will help to lessen the swelling. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling as well.
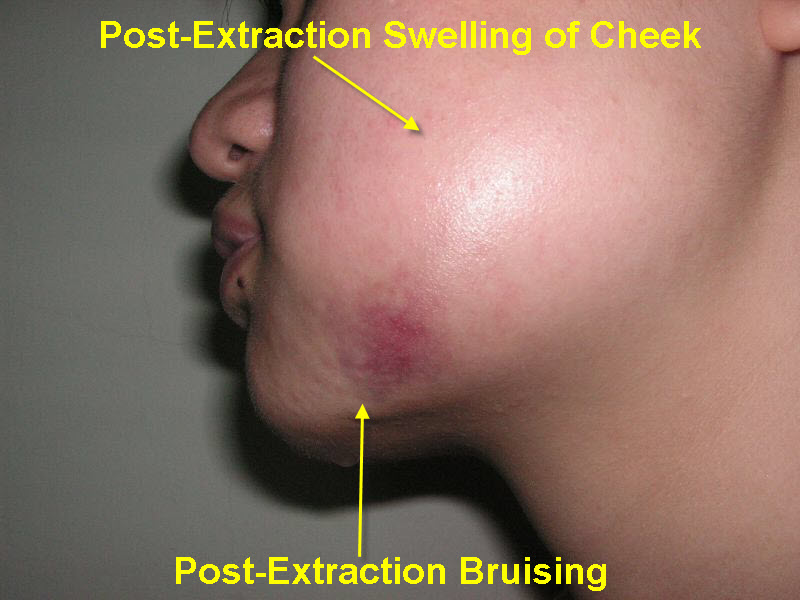
Bruising.
Some people are prone to bruise. Older people, people on aspirin or steroids will also bruise that much more easily. The bruising can look quite florid; this will eventually resolve but can take several weeks (in the worst cases).

Limitation of Mouth Opening (Trismus).
Limitation of Mouth Opening often the chewing muscles and the jaw joints are sore after the procedure so that mouth opening can be limited for the next few days. If you are unlucky enough to develop an infection afterwards in the socket, this can make the limited mouth opening worse and last for longer (up to a week).
Post-op Infection.
Post-op Infection. You may develop an infection in the socket after the operation. This tends to occur 2 – 4 days later and is characterised by a deep-seated throbbing pain, bad breath and an unpleasant taste in the mouth. This infection is more likely to occur if you are a smoker, are on the Contraceptive Pill, on drugs such as steroids and if bone has to be removed to facilitate tooth extraction.
If antibiotics are given, they are likely to react with alcohol and / or the Contraceptive Pill (that is, the ‘Pill’ will not be providing protection).
Adjacent Teeth.
The surrounding teeth may be sore after the extraction; they may even be slightly wobbly but the teeth should settle down with time. It is possible that the fillings or crowns of the surrounding teeth may come out, fracture or become loose. If this is the case, you will need to go back to your dentist to have these sorted out. Every effort will be
made to make sure this doesn’t happen. In very rare instances, the surrounding teeth may actually come out as well as the intended tooth.
Surgical Removal.
To ease the removal of teeth, it is sometimes necessary to cut the gum and/or remove bone from around the tooth. If this is the case, you can expect the extraction site to be more sore afterwards, the swelling to be greater and more likely to become infected. Hence, stronger painkillers are needed; use of icepacks necessary and antibiotics will probably be prescribed. The bone grows back to a greater extent. Care though will be taken not to be ‘wasteful’ in bone removal as this effects afterwards the provision of dentures, bridges and implants.
Numbness / Tingling / ‘Burning’ of the Lip, Chin and/or Tongue.
Numbness / Tingling / ‘Burning’ of the Lip, Chin and/or Tongue. The nerves that supply feeling to the tongue, lower lip and the chin run close to the root-ends of the lower molar teeth and exit onto the gum close to the roots of the premolars / bicuspids. There is a risk that when back lower teeth (wisdom teeth especially) are removed, these nerves can be crushed, bruised or stretched resulting in numbness (at the worse end of the scale) to altered sensation (at the other end of the scale) in the region of the lower lip, chin and/or tongue.
This nerve bruising tends to be temporary (rarely is it permanent) but ‘temporary’ can stretch from several days to several months. It is hard to predict who will get nerve bruising and if it will be temporary / permanent and if temporary, how long for.
Left Behind Tooth Tips.
In rare instances, the very ends of the teeth may be left behind.
In the lower jaw, this is done because in trying to remove these root tips, the nerve supplying feeling to the lip, chin & tongue may be damaged. If they are left behind, there is not likely to be any problems associated with this.
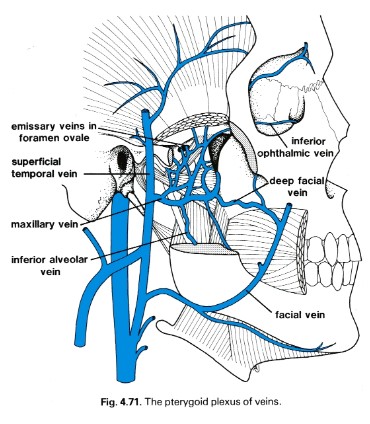
In the upper jaw, these root tips may stay where they are in the socket or may be pushed into the sinus or into a local blood vessel network (pterygoid plexus). If these tips are left behind in the socket, there is not likely to be any problems associated with this. However, if the root tips have gone out of the socket into the local anatomy, they will need to be recovered.
Bony Flakes.
Occasionally, bony flakes (sequestra) from the sockets of the extracted teeth can work their way loose and through the gums. These can be quite sore. They often work their way loose without any problems but may need to be teased out or even smoothed. If a number of teeth are removed at one go, the resulting gums may feel a bit rough. In many cases, the gums become less rough with time however, it may be necessary to smooth the underlying bone for this to happen.
Failure of Anasthesia.
in rare cases, the tooth can be difficult to ‘numb up’. This can be due to a number of reasons. The more common ones include inflammation ± infection associated with the tooth, anatomical differences & apprehension. If the tooth fails to ‘numb up’ then its removal will be rescheduled with antibiotic cover or perhaps done under sedation or even a GA.
Bleeding into Cheeks.
Swelling that does not resolve within a few days may be due to bleeding into the cheek. The cheek swelling will feel quite firm. Coupled with this, there may be limitation to mouth opening and bruising. Both the swelling, bruising and mouth opening will resolve with time.
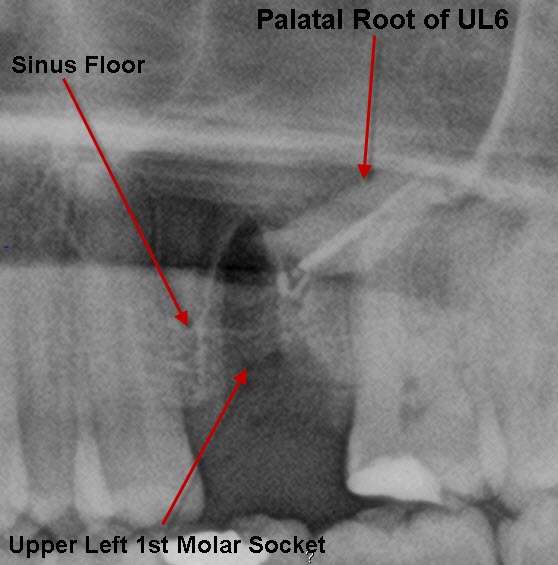
Mouth-Sinus Communications.
Mouth-Sinus Communications. Upper molar and premolar teeth often have their roots in close proximity to the sinus. In removing these teeth, there is a chance that a ‘hole’ can be made between the mouth & the sinus (this is sometimes not evident at the time of operation but may develop several weeks afterwards). If this ’hole’ persists or is left un-repaired, every time you drink, fluid can come out of the nose and you may develop a marked sinusitis. This ‘hole’ if small enough, can spontaneously close. It can be assisted in this by ‘cover plates’ that prevents food & fluids going into the sinus allowing the hole to close naturally. However, ‘holes’ above a certain size need to be surgically closed.
Mouth-Sinus Communications.
Mouth-Sinus Communications. Upper molar and premolar teeth often have their roots in close proximity to the sinus. In removing these teeth, there is a chance that a ‘hole’ can be made between the mouth & the sinus (this is sometimes not evident at the time of operation but may develop several weeks afterwards). If this ’hole’ persists or is left un-repaired, every time you drink, fluid can come out of the nose and you may develop a marked sinusitis. This ‘hole’ if small enough, can spontaneously close. It can be assisted in this by ‘cover plates’ that prevents food & fluids going into the sinus allowing the hole to close naturally. However, ‘holes’ above a certain size need to be surgically closed.
Fractured Tuberosity.
Fractured Tuberosity. The upper molars can, from time to time, be fused with the bone around them so that in removing the molar tooth, the bony socket within which the tooth sits (tuberosity) comes with it. This can make the mouth-sinus communication larger and sometimes, the adjacent teeth and their bony sockets comes attached with the extracted tooth.
Closure of the ‘hole’ is followed with antibiotics, painkillers & decongestants.
Nose-blowing is forbidden for a week afterwards (at least).
Prolonged Period of Disability.
Prolonged Pain.
Prolonged Limitation of Mouth Opening (Trismus).
Prolonged Bleeding from the Extraction Site.
Prolonged Swelling. Discomfort, swelling and œdema are normally considered inevitable consequences of wisdom tooth removal but as part of general improvement in patient care, all reasonable steps would have been taken to minimise them.
Excessive operative time, difficulty of extraction (such as bone removal) and flap retraction increase the swelling associated with surgery.
Periodontal Complications.
Systemic Medical / Surgical complications / Death during Operative / Post-Operative Period.
Complications associated with Local An?sthetic,
Sedation or General Anasthetic.
Development of Excessive Blood Clot / Bruising.
Development of excessive blood clot (h?matoma) in chewing muscles, tissue spaces etc may manifest itself on the face and slump into the submandibular region and then down the neck onto the chest.
Also, effects of blood clots being converted into scar tissue – prolonged trismus. H?matoma formation outwith the socket can occur and may require drainage.
Unscheduled Secondary Surgical Procedure.
Ludwig’s Angina.
his is a potentially fatal infection that involves the fascial spaces of the floor of the mouth and neck. Now rare but it still needs to be taken seriously.
Acute / Chronic / Local / Systemic Infection including Development of Osteomyelitis.
Persistence of / Development of New Pathology (eg. recurrent or residual cyst or tumour)
Sub-Cutaneous (Surgical) Emphysema.
Very rarely, air can enter the skin around the operation site and become trapped. This can lead to swelling, especially around the eyes or over the cheeks. This can be quite disconcerting however it slowly subsides and there is nothing really to worry about.
Post-Extraction Granuloma.
This complication occurs 4 – 5 days after the extraction of the tooth and is the result of the presence of a foreign body in the tooth socket e.g. amalgam remnants (from the tooth filling), bone chips, small tooth fragments, calculus etc. Foreign bodies irritate the area, so that post-extraction healing ceases and there is suppuration of the wound.
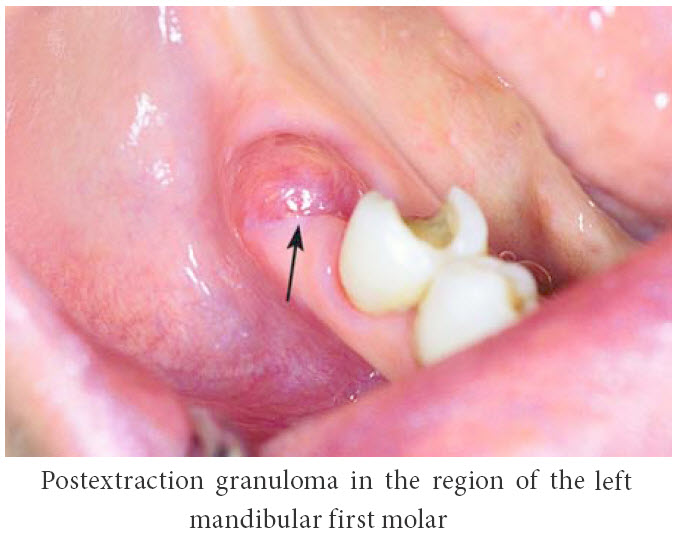
This complication is treated with debridement of the socket and removal of any / every causative agent.
Lingual Plate Fracture.
Lingual Plate Fracture. This is seen with:
- horizontally / mesially impacted lower wisdom teeth that have been partially erupted for awhile together with
- low-grade infection associated with them (such as pericoronitis or periodontitis)
- root forms that make the tooth more resistant to extraction
- large roots
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- horizontally / mesially impacted lower wisdom teeth that have been partially erupted for awhile together with
- low-grade infection associated with them (such as pericoronitis or periodontitis)
- root forms that make the tooth more resistant to extraction
- large roots
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- low-grade infection associated with them (such as pericoronitis or periodontitis)
- root forms that make the tooth more resistant to extraction
- large roots
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- root forms that make the tooth more resistant to extraction
- large roots
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- large roots
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- the sudden application of force
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- African origin (denser bone)
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- the more mature patient (sclerotic bone)
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- fusion of the tooth to the surrounding bone (ankylosis)
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
- the use of chisels / osteotomes, utilised in the decoronating of lower wisdom teeth (Lingual Split Technique used to ‘saucerise the socket’).
The plate fragment is often adherent to the wisdom tooth.
Dependent on its size, it can be dissected out. The socket will need to be ‘tidied up’ (the archaic term “wound toilet” is used). It is possible that the Lingual Nerve may be traumatised whilst this is being done. This will result in nerve damage that ranges from numbness of the tongue to ‘pins and needles’ or ‘burning’ of that side of the tongue as the extraction to loss of taste.
Introduction / Displacement of Tooth, Tooth Fragments or other Foreign Body / Bodies into Adjacent Anatomical Zones.
Jaw Dislocation.
Jaw Dislocation can be extremely uncomfortable having a lower molar tooth extracted, not because of pain at the surgical site but because of traction on the temporomandibular joints (TMJ) / jaw joints, consequent to the oral surgeon pushing down on the tooth with the extraction forceps. It is important that the surgeon fully supports the lower jaw during extractions in order to relieve stresses on the TMJ.
Where extractions are performed under General An?sthetic, it is all too easy to forget the TMJ. On completion of treatment, immediately prior to removing the throat pack, the oral surgeon should manipulate the lower jaw into centric occlusion to ensure that it is not dislocated (i.e. the lower jaw has gone back into its correct position). If it is not, then the dislocation should be reduced before the an?sthetic is reversed and the patient woken up.
Removal of wisdom teeth may cause / exacerbate a pre-existing TMJ problem. This complication is best prevented by allowing the patient to bite on a prop and rest every few minutes if the procedure is prolonged. If TMJ problems do occur following wisdom teeth removal or other oral surgical procedures, they must be treated in the normal way utilising
predominantly non-surgical modalities, such as rest, heat, muscle relaxants and possibly,Blood injection.
Removal of wisdom teeth may cause / exacerbate a pre-existing TMJ problem. This complication is best prevented by allowing the patient to bite on a prop and rest every few minutes if the procedure is prolonged. If TMJ problems do occur following wisdom teeth removal or other oral surgical procedures, they must be treated in the normal way utilising
predominantly non-surgical modalities, such as rest, heat, muscle relaxants and possibly,Blood injection.
predominantly non-surgical modalities, such as rest, heat, muscle relaxants and possibly,Blood injection.
Exposure of an Inappropriate / Unplanned Operative Site (eg. incorrect side)
Extraction of the Wrong Tooth.
Fractured Upper / Lower Jaw secondary to Tooth Removal.
Fracture / Failure of Instrument with Retention of Instrument Fragment within Bone / Soft Tissue.
Soft Tissue Damage.
Aspiration.
All tooth extractions carry the risk of aspiration (the tooth is inhaled). The use of sedation compromises the protective reflexes of the airway. Aspiration is usually the result of a patient coughing or gagging.