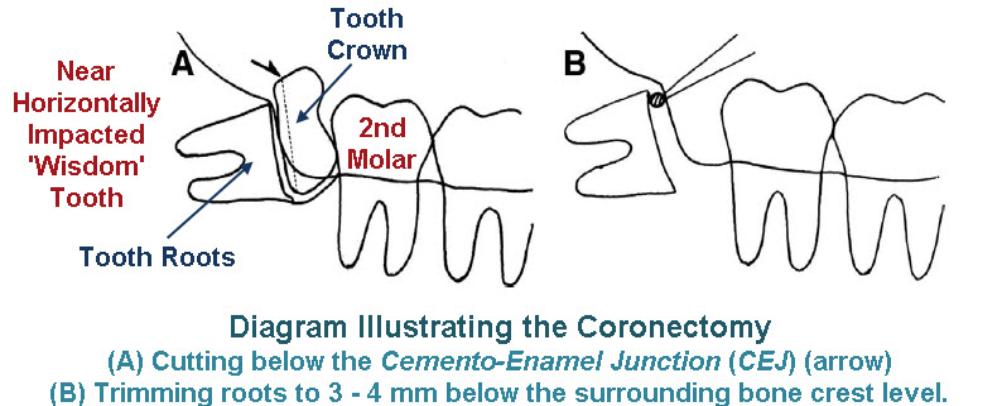
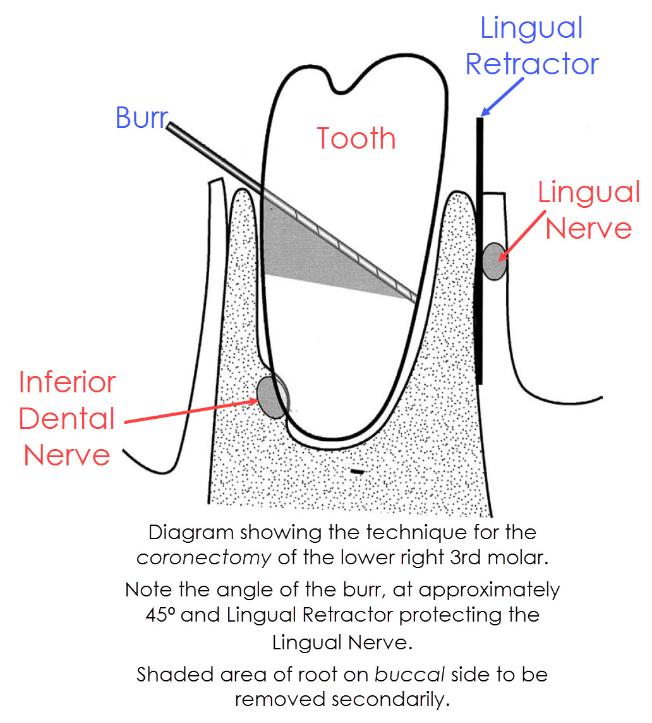
Coronectomy is the removal of the crown of a tooth, leaving the roots in situ.
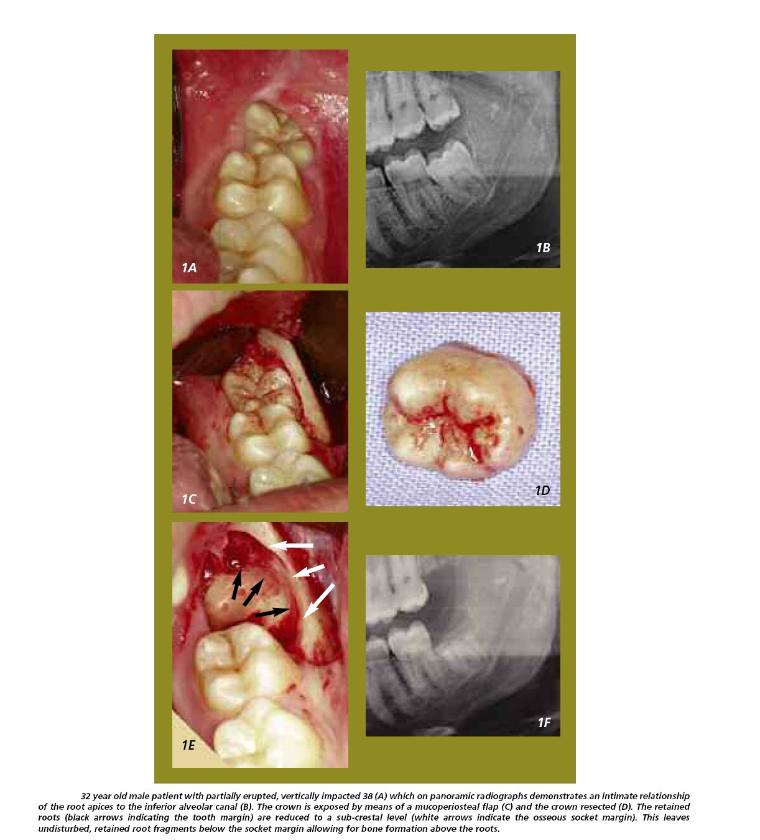
When applied to a lower wisdom tooth or any lower unerupted posterior tooth, it is a procedure used to avoid damage to the Inferior Alveolar Nerve (IAN) (the nerve that supplies feeling / sensation to the lip and chin) when the X-ray has suggested an intimate relationship between the roots of the lower wisdom tooth and the IAN (the intimacy of the tooth roots to the nerve canal can be confirmed with the use of a Cone Beam CT scan [CBCT]).
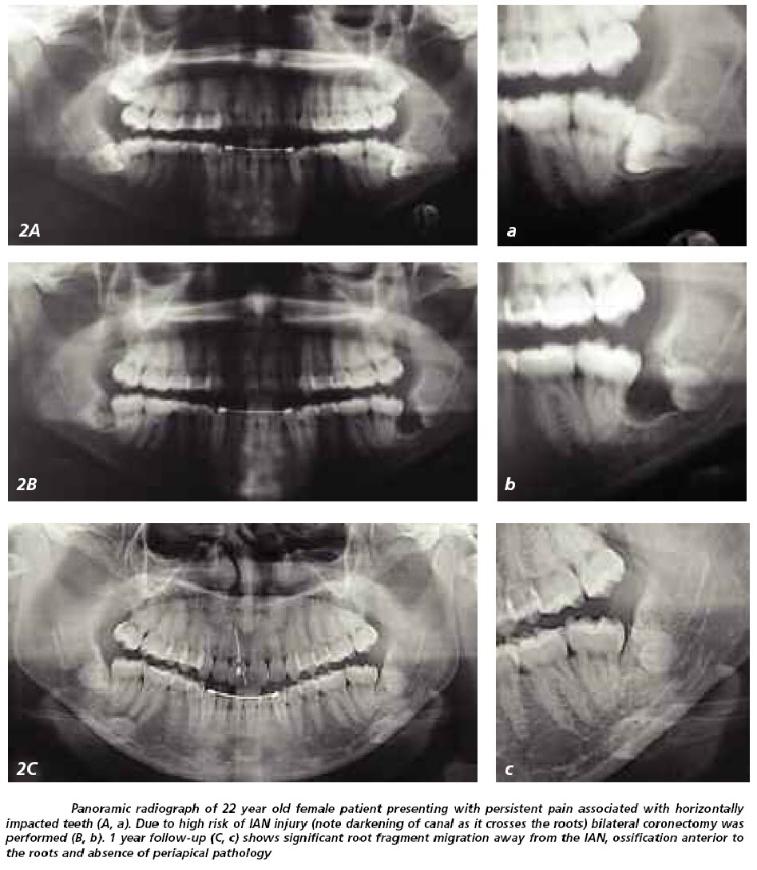
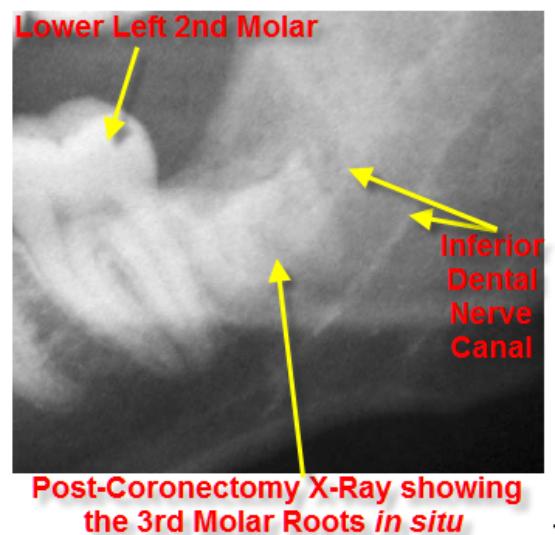
The expectation, after removing the top of the tooth, is that the roots will remain in place and eventually sealed with bone.
Roots encased in bone can remain buried in the jaw for years and rarely cause problems.
Coronectomy of lower molars is NOT carried out in the following situations:
- Wisdom tooth roots are not touching the IAN canal
- Wisdom tooth with either active root tip infection or decay in the crown of the tooth (which extends to the pulp)
- Active periodontal disease in the region of the wisdom tooth and the tooth in front of the wisdom tooth
- Pre-existing numbness of the IAN
- Pre-existing mobility of the tooth as any retained roots may act as a mobile foreign body and become a nidus for infection / migration
- Teeth that are horizontally impacted along the course of the IAN as sectioning the tooth crown could endanger the IAN
- Systemic condition predisposing to local infection such as diabetes, AIDS and concurrent chemo-therapy / radio-therapy
- Local factors predisposing to infection such as metabolic bone diseases (e.g. fibrous dysplasia), history of radio-therapy to the lower jaw
- Where it would not be possible to remove all the enamel (retention of enamel seems to be associated with a higher failure rate)
- Where the 2nd molars will be moved distally in orthodontic treatment or orthognathic surgery on the mandible is being considered.
- Where the tooth is associated with tumours or large cysts
The medico-legal landscape of consent has been shaped by a number of cases, such as Chester v Afshar [2004], Montgomery v Lanarkshire Health Board [2015], Duce v Worcestershire Acute Hospitals NHS Trust [2018] amongst others, so that it is more patient-centred.
Many of the legal claims in surgical (& medical) cases occur as a result of “failure to warn”, i.e. lack of adequately documented and appropriate consent.
A pre-requisite for obtaining consent for a surgical (medical / dental) procedure from a patient, is a full exchange of information regarding any risks, drawbacks and limitations of the proposed treatment and any alternatives to it (even non-treatment).
The clinicians should provide the patient with as much information as is appropriate and relevant, that it should be in terms the patient understands & the risks should be personalised for that individual patient. Also, there should be enough time for the patient to understand the information given and get a second opinion if needs be.
The following list of warnings regarding coronectomy is neither exhaustive nor is it predictive.
You are to have a tooth decoronated. You can expect the following:
Coronectomy / Intentional Partial Odontectomy Specific Warnings:
Roots inadvertently removed at the time of attempted coronectomy.
When the crown of the tooth is mobilised, the roots (if the crown is still attached to them) may become mobile as well. This ranges from 3 – 9%. If the roots are mobile, we are obliged to remove them and there is obviously the risk to the IAN (which this procedure was trying to avoid). This is more likely to happen if the roots are conical in shape.
Incomplete Crown Removal (link to annotated picture).
Not being able to visualize the root surface is a common problem with disto-angular impactions and makes root finishing difficult. This may mean that all the enamel has not been removed. Retained enamel or spicules of enamel can cause irritation to the overlying gum or, as the enamel acts as foreign body, increases the chances of infection of the unhealed socket.
Numbness of Chin, Lip ± Tongue.
The Inferior Alveolar & Lingual Nerves may still be damaged during the procedure resulting in numbness affecting the tongue ± the chin and lower lip. The numbness of the tongue seems to be quite short-lived and has a low incidence. The numbness of the chin ± lip tended to occur when on attempting the coronectomy, the roots were found to be mobile and had to be removed
Root Migration.
Subsequent migration of the roots away from the IAN occurred in 14 – 81% of cases. The roots seem to move the most during the first 6 months post-coronectomy, with a typical distance of 2 – 3mm away from the IAN. Root migration halts as the bone regenerates and remodels.
Later Removal of Roots.
This can happen in up to a 2 – 6% of cases. If the roots irritate overlying tissues or the adjacent tooth or otherwise become symptomatic, they may need to be removed. Even though a 2nd surgery would be needed, the possibility of nerve damage should be negligible since the roots would have migrated away from its original resting place next to the IAN. Since the purpose of the coronectomy is to avoid this damage, this goal would have been accomplished even though a 2nd surgical procedure was necessary to remove the remaining root.
General Surgical Warnings:
Pain.
As it is a surgical procedure, there will be soreness after the tooth removal. This can last for several days. Painkillers such as ibuprofen, paracetamol, Solpadeine or Nurofen Plus are very effective. Obviously, the painkiller you use is dependent on your medical history & the ease of the operation. The pain can take awhile to settle down – it is not so much the pain of a tooth extraction but of a tooth that has been irreversibly traumatised and the tooth’s pain is that of the tooth dying – this can be prolonged.
Swelling.
There will be swelling afterwards. This can last up to a week. Use of an icepack or a bag of frozen peas pressed against the cheek adjacent to the coronectomy site will help to decrease the swelling. Avoidance in the first few hours post-op, of alcohol, exercise or hot foods / drinks will decrease the degree of swelling that will develop.
Some people are prone to bruise. Older people, people on aspirin or steroids will also bruise that much more easily. The bruising can look quite florid; this will eventually resolve but can take several weeks (in the worst cases).
Swelling that does not resolve within a few days may be due to bleeding into the cheek.
The cheek swelling will feel quite firm. Coupled with this, there may be limitation to mouth opening and bruising. Both the swelling, bruising and mouth opening will resolve with time.
Stitches.
The coronectomy site will often be closed with stitches. These dissolve and will ‘fall out’ within 10 – 14 days.
Limited Mouth Opening.
Often the chewing muscles and the jaw joints are sore after the procedure so that mouth opening can be limited for the next few days. If you are unlucky enough to develop an infection afterwards, this can make the limited mouth opening worse and last for longer (up to a week or so).
Post-op Infection.
You may develop an infection in the socket after the operation. This tends to occur 2 – 4 days later and is characterised by a deep-seated throbbing pain, bad breath and an unpleasant taste in the mouth. This infection is more likely to occur if you are a smoker, are on the contraceptive pill, on drugs such as steroids and if bone has to be removed to facilitate tooth extraction.
If antibiotics are given, they are likely to react with alcohol and / or the Contraceptive Pill (that is, the ‘Pill’ will not be providing protection).
Surrounding Teeth.
The surrounding teeth may be sore after the coronectomy; they may even be slightly wobbly but the teeth should settle down with time. It is possible that the fillings or crowns of the surrounding teeth may come out, fracture or become loose. If this is the case, you will need to go back to your dentist / Oral Surgeon to have these sorted out. Every effort will be made to make sure this doesn’t happen.
Damage to the lower 2nd molar (that is, the tooth in front of the wisdom tooth) has been reported, which likely occurs when removing all enamel from mesio-angular impacted wisdom teeth and there is limited access and visibility of the operation site.
Failure of Anaesthesia.
In rare cases, the tooth can be difficult to ‘numb up’. This can be due to a number of reasons. The more common ones include inflammation ± infection associated with the tooth, anatomical differences & apprehension. If the tooth fails to ‘numb up’ then its removal will be rescheduled with antibiotic cover or perhaps done under sedation or even a GA.
Useful Articles & Websites
J Oral Maxillofac Surg 2004. Coronectomy: A Technique to Protect the Inferior Alveolar Nerve